
Get health insurance for my business
Securing health insurance for your business is a pivotal step in ensuring the well-being of your employees and the overall success of your company. Offering comprehensive health coverage not only attracts and retains top talent but also fosters a productive and satisfied workforce. Navigating the landscape of business health insurance can be complex, but with the right information and guidance, you can make informed decisions that align with your company's needs and budget.
Understanding Business Health Insurance
What is Business Health Insurance?
Business health insurance, also known as group health insurance, is a type of medical coverage offered by employers to their employees and, in some cases, their dependents. Unlike individual health insurance plans, business health insurance policies are designed to cover multiple employees under a single plan, often resulting in more affordable premiums and broader coverage options.
Definition and Purpose
The primary purpose of business health insurance is to provide employees with access to quality healthcare, ensuring that they can receive medical treatment when needed without facing financial hardship. By offering health insurance, businesses not only support their employees’ well-being but also benefit from a more stable and productive workforce.
Benefits for Employers and Employees
For Employers:
- Attract and Retain Talent – A competitive benefits package, including health insurance, helps businesses stand out in the job market.
- Tax Advantages – Employers may qualify for tax credits and deductions for providing health coverage.
- Increased Productivity – Healthy employees are more engaged, take fewer sick days, and contribute more effectively to the business.
- Improved Employee Satisfaction – Offering health benefits enhances job satisfaction and reduces turnover rates.
For Employees:
- Access to Affordable Healthcare – Employees receive medical coverage at lower costs than individual plans.
- Preventive Care and Wellness Programs – Many plans cover routine check-ups, vaccinations, and screenings at no additional cost.
- Financial Security – Health insurance helps mitigate unexpected medical expenses, reducing out-of-pocket costs.
- Coverage for Dependents – Employees can extend coverage to their spouses and children, ensuring their family’s health needs are met.
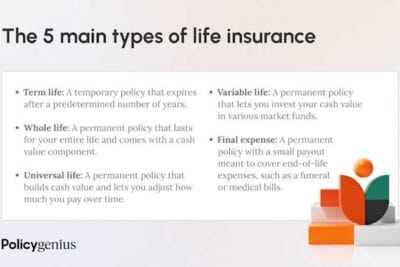
Types of Health Insurance Plans
Employers can choose from various health insurance plans, each with distinct structures, benefits, and cost considerations. The right plan depends on factors such as business size, budget, employee needs, and network preferences.
1. Health Maintenance Organization (HMO)
A Health Maintenance Organization (HMO) is a type of health insurance plan that requires members to receive care from a specific network of doctors, hospitals, and healthcare providers.
Key Features:
✔ Requires a primary care physician (PCP) to coordinate all healthcare services.
✔ Referrals are needed to see specialists.
✔ Typically lower premiums and out-of-pocket costs, but less flexibility in choosing providers.
✔ Focuses on preventive care and wellness programs to keep employees healthy.
Best for: Businesses looking for cost-effective plans with a structured care approach.
2. Preferred Provider Organization (PPO)
A Preferred Provider Organization (PPO) plan offers more flexibility in choosing healthcare providers and does not require a primary care physician (PCP) or referrals for specialists.
Key Features:
✔ Employees can see any doctor or specialist, but they save money by using in-network providers.
✔ Higher premiums and out-of-pocket costs compared to HMO plans.
✔ Greater flexibility in choosing doctors and hospitals.
✔ Covers out-of-network care, though at a higher cost.
Best for: Businesses that want to provide employees with more healthcare provider options while maintaining coverage flexibility.
3. Exclusive Provider Organization (EPO)
An Exclusive Provider Organization (EPO) plan is similar to an HMO, but it does not require a referral to see specialists.
Key Features:
✔ Employees must use in-network providers, except in emergencies.
✔ Lower premiums than PPO plans.
✔ No referrals needed for specialists, making access to care faster and easier.
✔ Ideal for businesses that want lower costs without sacrificing provider choice entirely.
Best for: Businesses looking for affordable plans with a balance of cost savings and specialist access.
4. Point of Service (POS)
A Point of Service (POS) plan combines features of HMO and PPO plans, providing flexibility while still requiring a primary care physician (PCP).
Key Features:
✔ Employees must choose a PCP who coordinates their care.
✔ Referrals are required for specialists.
✔ Allows out-of-network care, but at a higher cost.
✔ Premiums and out-of-pocket costs fall between HMO and PPO plans.
Best for: Businesses that want more provider choices than an HMO while keeping costs relatively lower than a PPO.
5. High-Deductible Health Plans (HDHP) with Health Savings Accounts (HSA)
A High-Deductible Health Plan (HDHP) is a cost-effective insurance plan with lower premiums but higher deductibles. Employees can pair these plans with a Health Savings Account (HSA), which allows them to save money tax-free for medical expenses.
Key Features:
✔ Lower monthly premiums, making it a cost-saving option for businesses.
✔ Higher deductibles, meaning employees must pay more out-of-pocket before coverage kicks in.
✔ HSAs allow employees to save pre-tax dollars for healthcare expenses, including deductibles, copayments, and prescriptions.
✔ Encourages employees to be more mindful of their healthcare spending.
Best for: Businesses that want to lower insurance costs while providing employees with tax-advantaged savings for healthcare expenses.
Choosing the Right Plan for Your Business
When selecting a business health insurance plan, employers should consider:
✔ Company size and budget – What can your business afford while maintaining quality benefits?
✔ Employee demographics and healthcare needs – Do employees prefer lower premiums, or do they need flexible provider options?
✔ Regulatory requirements – Does your business meet ACA mandates and state regulations?
✔ Provider networks and accessibility – Are healthcare providers conveniently located for employees?
✔ Potential tax benefits – Can the plan help maximize tax savings for both employer and employees?
Providing health insurance for your employees is one of the most valuable investments your business can make. Not only does it improve employee well-being, but it also enhances workplace satisfaction and ensures your company remains competitive in attracting and retaining top talent.
Assessing Your Business Needs
Selecting the right health insurance plan for your business requires a comprehensive assessment of your workforce’s demographics, healthcare needs, and financial constraints. By understanding the unique characteristics of your employees and aligning them with a well-structured budget, businesses can ensure they provide adequate, cost-effective, and beneficial health coverage.
Evaluating Employee Demographics
To choose the most suitable business health insurance plan, it is crucial to assess the specific needs and characteristics of your workforce. Employee demographics—such as age, family status, and health preferences—play a significant role in determining the type of coverage that will be most beneficial.
1. Age Distribution
The age range of your employees can significantly impact their healthcare needs and preferences.
- Younger employees (20s – early 30s)
✔ Typically prioritize lower-cost plans with minimal coverage, as they may have fewer medical needs.
✔ More likely to choose High-Deductible Health Plans (HDHPs) with Health Savings Accounts (HSAs) to save on premiums while securing tax-free medical savings.
✔ May prefer telehealth options and wellness programs over traditional in-person care. - Middle-aged employees (30s – 50s)
✔ More likely to seek comprehensive plans that include preventive care, specialist visits, and family coverage.
✔ Often require coverage for chronic conditions (e.g., hypertension, diabetes).
✔ May prioritize Preferred Provider Organization (PPO) or Exclusive Provider Organization (EPO) plans for broader provider access. - Older employees (50s and above)
✔ More likely to require specialist care, prescription medications, and chronic disease management.
✔ May favor low-deductible plans with robust preventive and long-term care coverage.
✔ Often seek plans with wellness and disease management programs to support overall health.
2. Family Status
Understanding the family dynamics of your employees can help determine whether individual or family plans should be prioritized.
- Single employees with no dependents
✔ Typically opt for individual coverage with lower premiums and deductibles.
✔ May not require maternity or pediatric care benefits. - Employees with families
✔ Require plans that offer comprehensive family coverage, including maternity, pediatric, and dental care.
✔ Seek affordable dependent coverage with low copayments for routine visits.
✔ More likely to choose PPO or POS plans to accommodate specialist visits for children and spouses. - Employees nearing retirement
✔ May require retirement transition plans, such as Medicare supplemental insurance.
✔ May prioritize long-term care benefits and prescription drug coverage.
3. Health Needs and Preferences
A business’s workforce is diverse, and each employee may have different health priorities and expectations from their employer’s health plan.
- Employees with chronic conditions (e.g., diabetes, heart disease, asthma)
✔ Require consistent access to specialists and prescription drug coverage.
✔ Benefit from wellness programs, telemedicine, and preventive screenings.
✔ Best suited for PPO or HMO plans with comprehensive coverage and lower out-of-pocket costs. - Employees who prioritize mental health care
✔ Look for plans that cover mental health services, therapy, and counseling.
✔ Prefer coverage that includes telehealth and virtual mental health services. - Employees with active lifestyles
✔ Seek preventive care and fitness-related benefits.
✔ May benefit from wellness incentives, gym memberships, and routine screenings.
Exploring Coverage Options
Choosing the right health insurance for your business involves exploring different coverage options that align with your company's size, budget, and employee needs. Employers can select from government-backed programs like the Small Business Health Options Program (SHOP), private insurance marketplaces, and self-funded plans. Each option comes with its own set of benefits, risks, and administrative requirements.
Small Business Health Options Program (SHOP)
The Small Business Health Options Program (SHOP) is a government-supported insurance marketplace designed to help small businesses (with fewer than 50 full-time employees) provide health coverage to their workforce. SHOP plans are available through the federal or state marketplace, depending on your location.
1. Eligibility Criteria
To qualify for SHOP insurance, businesses must meet the following requirements:
✔ Business Size – Must have 1 to 50 full-time equivalent (FTE) employees (some states allow up to 100 employees).
✔ Employee Participation – A minimum percentage of employees (usually 70%) must enroll in the plan.
✔ Employer Contributions – Employers must cover at least 50% of the premium costs for full-time employees.
✔ Valid Business Status – The company must be legally registered and operate within the U.S..
2. Benefits of Using SHOP
Employers who choose SHOP enjoy multiple benefits:
✔ Tax Credits for Small Businesses – Businesses with fewer than 25 employees and an average salary of $56,000 or less per year (as of 2024) may qualify for the Small Business Health Care Tax Credit, covering up to 50% of premium costs.
✔ Flexible Plan Options – Employers can offer multiple plan choices, allowing employees to select the best fit for their needs.
✔ No Restrictions on Pre-existing Conditions – Ensures that all employees, regardless of health status, receive coverage.
✔ Streamlined Enrollment Process – Employers can sign up directly through HealthCare.gov or a state marketplace.
3. Enrollment Process
Employers can enroll in a SHOP plan at any time during the year. The process includes:
- Determine Eligibility – Use the SHOP eligibility checker on HealthCare.gov.
- Compare Plans – Browse and compare available SHOP plans based on cost, coverage, and provider networks.
- Select a Plan – Choose a plan that meets your business needs and decide on employer contribution levels.
- Enroll Online or Through a Broker – Sign up through the federal or state marketplace, or work with a licensed insurance broker.
- Manage Coverage – Employers can update employee lists, adjust contributions, or switch plans during open enrollment or qualifying life events.
Private Health Insurance Marketplaces
Employers who do not qualify for SHOP or prefer more flexible options can explore private health insurance marketplaces. These are insurance providers, brokers, or third-party exchanges that offer customizable group health plans.
1. Comparing Plans from Various Insurers
When selecting a private insurance plan, consider the following:
✔ Premium Costs – Compare monthly premiums based on coverage level.
✔ Deductibles & Out-of-Pocket Costs – Ensure the plan offers an affordable balance between deductibles, copayments, and coinsurance.
✔ Network Size – Check if the plan includes hospitals and providers within your region.
✔ Prescription Drug Coverage – Verify the formulary (list of covered medications), especially for employees who require ongoing prescriptions.
✔ Additional Benefits – Some plans offer wellness programs, telemedicine services, or dental/vision coverage.
2. Advantages of Working with Insurance Brokers
Using a licensed health insurance broker can simplify the plan selection process by providing:
✔ Personalized Plan Recommendations – Brokers assess your business needs and suggest the most suitable plans.
✔ Cost Comparison Across Insurers – They compare multiple insurers to find the best price-to-coverage ratio.
✔ Assistance with Enrollment & Compliance – Brokers help businesses navigate legal requirements, paperwork, and claims administration.
✔ Ongoing Support – They assist with renewals, plan modifications, and employee education.
Brokers are often paid by insurance companies, meaning their services are free for businesses—making them a cost-effective way to navigate the complex health insurance market.
Self-Funded Health Plans
Self-funded (or self-insured) health plans allow employers to pay employee medical claims directly, rather than purchasing a traditional insurance policy. This approach can be cost-effective but also comes with higher financial risks.
1. Overview and Benefits
With a self-funded plan, the employer assumes responsibility for paying employee healthcare costs rather than paying monthly premiums to an insurer.
Key Benefits:
✔ Lower Costs Over Time – Businesses save on insurance premiums and administrative fees.
✔ Customization – Employers can tailor coverage to meet specific employee needs.
✔ Cash Flow Control – Instead of paying fixed monthly premiums, businesses only pay for actual medical expenses.
✔ Tax Advantages – Self-insured employers avoid state health insurance premium taxes.
✔ Access to Claims Data – Businesses gain better insight into employee healthcare usage to adjust benefits accordingly.
Best for: Mid-size and large businesses that have predictable healthcare costs and want greater control over employee benefits.
2. Risks and Considerations
Despite cost-saving potential, self-funded plans carry financial risks that businesses must evaluate:
✔ Unpredictable Claims Costs – High medical expenses can drastically impact cash flow.
✔ Compliance Challenges – Employers must manage federal regulations (e.g., ERISA, ACA, COBRA).
✔ Potential Legal Liabilities – Failure to properly fund claims can result in penalties or lawsuits.
✔ Administrative Burden – Requires third-party administrators (TPAs) to handle claims processing and compliance.
To mitigate financial risks, businesses often purchase:
- Stop-Loss Insurance – Protects against catastrophic claims by reimbursing expenses above a set threshold.
- Third-Party Administrative Services – Helps manage claims, process paperwork, and handle compliance matters.
3. Legal and Administrative Requirements
Employers offering self-funded plans must comply with several federal regulations:
✔ Employee Retirement Income Security Act (ERISA) – Requires detailed reporting and fiduciary responsibilities.
✔ Affordable Care Act (ACA) Compliance – Self-insured plans must cover essential health benefits and comply with reporting mandates.
✔ COBRA Coverage – Businesses with 20 or more employees must offer continuation coverage for former employees.
✔ HIPAA Privacy & Security Rules – Employers handling medical claims must safeguard employee health information.
Self-funded plans demand a strong financial strategy, legal compliance, and efficient administration, making them a viable option for businesses prepared to handle the added responsibility.
Legal Requirements and Compliance
Ensuring compliance with health insurance regulations is a crucial responsibility for businesses offering coverage to employees. Federal and state laws govern employer obligations, reporting requirements, and potential penalties for non-compliance. The Affordable Care Act (ACA) establishes key mandates that businesses must follow, while state-specific regulations can impose additional coverage requirements and benefits.
Affordable Care Act (ACA) Mandates
The Affordable Care Act (ACA), enacted in 2010, introduced comprehensive reforms aimed at expanding healthcare access, improving coverage quality, and ensuring affordability. Under the ACA, businesses with a certain number of employees are required to offer health insurance or face potential penalties.
1. Employer Shared Responsibility Provisions (ESRP)
Under the Employer Mandate, Applicable Large Employers (ALEs)—those with 50 or more full-time equivalent (FTE) employees—must provide affordable, minimum essential coverage (MEC) to at least 95% of full-time employees and their dependents or face penalties.
Key requirements for ALEs:
✔ Coverage must be affordable – Employee contributions for the lowest-cost plan cannot exceed 9.12% of their household income (as of 2023).
✔ Minimum essential coverage (MEC) is required – Plans must cover essential health benefits, including preventive care, emergency services, and prescription drugs.
✔ Coverage must meet minimum value (MV) standards – The plan must cover at least 60% of total healthcare costs.
If an employer fails to meet these requirements, they may face significant financial penalties under Section 4980H of the Internal Revenue Code.
2. Reporting Obligations
Employers must file annual reports with the IRS and provide statements to employees detailing their health insurance coverage.
✔ Form 1095-C – Required for ALEs; reports whether health insurance was offered to full-time employees.
✔ Form 1094-C – Summary report submitted to the IRS with details on employer coverage.
✔ Deadlines – Generally due in January (employee forms) and February/March (IRS filings) of the following year.
Failure to comply with reporting obligations can result in penalties of up to $290 per form (as of 2023).
3. Penalties for Non-Compliance
Employers who fail to offer ACA-compliant coverage or do not meet reporting requirements may face penalties.
Common ACA penalties include:
- 4980H(a) Penalty – Failure to Offer Coverage
- If an ALE does not offer coverage to at least 95% of full-time employees and at least one employee receives premium tax credits, the employer faces a penalty of $2,880 per full-time employee (minus the first 30 employees) in 2023.
- 4980H(b) Penalty – Unaffordable or Non-Qualifying Coverage
- If an ALE offers coverage that is either not affordable or does not meet minimum value, and an employee receives premium tax credits, the employer is fined $4,320 per affected employee in 2023.
- Failure to File or Furnish Forms 1095-C and 1094-C
- Employers who fail to file or furnish required ACA forms may incur penalties of up to $580 per form (capped at $3.5 million annually, depending on business size).
To avoid penalties, businesses should:
✔ Ensure full-time employees are offered compliant coverage.
✔ Review affordability standards and make adjustments as necessary.
✔ File all required ACA reports accurately and on time.
State-Specific Regulations
In addition to federal ACA mandates, individual states may impose additional regulations that affect employer-sponsored health insurance. Some states mandate expanded coverage, reporting obligations, or tax incentives beyond federal requirements.
1. Variations in Coverage Requirements
Many states go beyond ACA requirements to offer additional benefits, particularly in areas like mental health, fertility treatments, and telemedicine.
✔ California, New York, and Massachusetts – Require insurers to cover fertility treatments, including in vitro fertilization (IVF).
✔ Oregon and Illinois – Mandate expanded mental health and substance abuse coverage beyond ACA standards.
✔ Washington and Maryland – Require coverage of telehealth services at the same rate as in-person visits.
Employers operating in multiple states must ensure their health plans comply with state-specific mandates in each location.
2. Additional Mandates and Benefits
State-Individual Mandates
Although the federal individual mandate (which required individuals to have insurance or pay a penalty) was eliminated in 2019, some states have enacted their own individual mandates, impacting employer-sponsored insurance.
✔ California, Massachusetts, New Jersey, Rhode Island, Vermont, and the District of Columbia require residents to maintain health coverage.
✔ Employers may need to report employee coverage status to state agencies in these states.
State-Level Small Business Incentives
Some states offer tax credits and subsidies to encourage small businesses to provide employee health insurance.
✔ New York – Offers tax credits to small businesses that enroll in the state’s marketplace plan.
✔ Minnesota – Provides reinsurance programs that reduce employer premium costs.
✔ Hawaii – Requires employers to offer health insurance to employees working 20+ hours per week, a stricter standard than the ACA.
3. Compliance Strategies for Multi-State Employers
Employers with a national workforce must ensure state-specific compliance by:
✔ Working with a licensed insurance broker or legal consultant who understands state regulations.
✔ Customizing health plans to meet varying state-level coverage requirements.
✔ Tracking reporting deadlines in states with individual mandates.
✔ Reviewing local tax incentives to take advantage of cost-saving programs.
Key Takeaways for Employers
✔ All businesses with 50+ full-time employees must comply with ACA mandates to avoid financial penalties.
✔ Health plans must be affordable and meet minimum essential coverage (MEC) and minimum value (MV) standards.
✔ Employers must file IRS reports (Forms 1095-C & 1094-C) to demonstrate compliance.
✔ State-specific health insurance laws vary, requiring multi-state employers to adjust plans accordingly.
✔ Failure to comply with ACA or state regulations can result in substantial fines and penalties.
Implementing a Health Insurance Plan
Once you’ve selected the right health insurance plan, the next step is implementing it effectively. Proper implementation involves choosing the best coverage option, communicating benefits to employees, and managing enrollment efficiently. A well-structured approach ensures that employees understand their options and can maximize their benefits, while the company remains compliant with regulations and cost-efficient.
Selecting the Right Plan
Choosing the best health insurance plan for your business requires a careful evaluation of coverage options, network availability, and overall costs. Employers must balance quality healthcare access with financial sustainability.
1. Comparing Coverage Options
When evaluating different health insurance plans, consider the following key factors:
✔ Coverage Levels – Does the plan offer comprehensive benefits, including preventive care, specialist visits, prescription drugs, and hospitalization?
✔ Premium Costs – How much will employers and employees need to contribute monthly?
✔ Deductibles and Out-of-Pocket Costs – Are there high deductibles or affordable copayments?
✔ Employer Contribution – What percentage of the premium cost will the employer cover?
✔ Employee Needs – Does the plan align with employee demographics, family status, and common medical conditions?
Comparing Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), Exclusive Provider Organization (EPO), and High-Deductible Health Plans (HDHP) with Health Savings Accounts (HSA) is essential to determine the best fit for your business.
2. Network Considerations
The provider network is a critical component of any health plan, as it determines where employees can receive medical care.
✔ In-Network vs. Out-of-Network Providers – HMO and EPO plans require employees to see in-network doctors, while PPO and POS plans offer out-of-network options at higher costs.
✔ Primary Care Physician (PCP) Requirement – Some plans mandate PCPs and referrals for specialists, while others offer direct specialist access.
✔ Hospital and Specialist Access – Check if major hospitals and preferred specialists are included in the network.
✔ Telemedicine Services – Does the plan offer virtual healthcare consultations for convenience and affordability?
3. Balancing Cost and Benefits
A well-structured health plan should balance affordability and comprehensive care.
✔ Affordable Premiums vs. High Deductibles – HDHPs offer lower premiums but require employees to pay higher deductibles before coverage kicks in.
✔ Wellness Incentives – Some plans provide discounts for gym memberships, smoking cessation, or weight loss programs.
✔ Prescription Drug Coverage – Ensure essential medications are covered at reasonable costs.
✔ Flexible Spending Accounts (FSAs) & Health Savings Accounts (HSAs) – These allow employees to save pre-tax money for medical expenses.
Employers should work with insurance brokers or benefits consultants to navigate these choices and find the best plan that meets business goals and employee needs.
Communicating with Employees
Once a health plan is selected, effective communication is key to ensuring employees understand their benefits and make informed choices.
1. Educating Staff About Plan Choices
Many employees struggle to understand health insurance terminology and benefits. Employers should provide clear, accessible resources to educate staff on:
✔ Plan Types and Differences – Explain HMO, PPO, EPO, and HDHP options.
✔ Coverage Details – Break down what’s covered, copays, deductibles, and out-of-pocket maximums.
✔ How to Choose the Right Plan – Help employees match their healthcare needs with the most suitable plan.
✔ Additional Benefits – Inform employees about telemedicine, mental health coverage, wellness incentives, and preventive care services.
Employers can conduct in-person meetings, webinars, or Q&A sessions to improve understanding and address concerns.
2. Enrollment Periods and Procedures
Employees need to be aware of enrollment deadlines and their responsibilities when signing up for health insurance.
✔ Open Enrollment Periods – Occur annually, typically between November and December, for coverage starting the following year.
✔ Special Enrollment Periods (SEPs) – Employees can enroll outside of open enrollment if they experience qualifying life events, such as:
- Marriage or divorce
- Birth or adoption of a child
- Loss of previous health coverage
- Relocation to a new coverage area
✔ New Hire Enrollment – Employers should outline how and when new employees can enroll.
✔ How to Enroll – Provide step-by-step instructions for online portals, paper forms, or HR department submissions.
3. Resources for Ongoing Support
To help employees navigate their health benefits throughout the year, employers should offer:
✔ HR Support Teams – Dedicated personnel to assist with benefits questions and claims issues.
✔ Digital Portals – Online platforms where employees can manage benefits, access policy details, and track claims.
✔ Helplines & Chat Support – Many insurance providers offer 24/7 customer service to resolve coverage and claim disputes.
✔ Annual Benefits Review Sessions – Regularly scheduled meetings to educate employees on updates and changes.
Proper communication ensures employees feel confident in their healthcare choices, leading to higher satisfaction and reduced administrative confusion.
Managing Enrollment and Administration
Efficiently handling health insurance enrollment and benefits management requires technology, compliance, and proper claims handling.
1. Utilizing Technology for Benefits Management
Employers can streamline health benefits management through digital tools and HR software.
✔ HR Benefits Platforms – Centralized systems (e.g., Gusto, Zenefits, ADP) for tracking enrollments, payroll deductions, and policy details.
✔ Employee Self-Service Portals – Employees can select plans, update personal information, and manage claims online.
✔ Automated Enrollment & Notifications – Ensures employees don’t miss deadlines or required paperwork.
✔ Integration with Payroll Systems – Seamlessly manages deductions and employer contributions.
Using technology reduces errors, saves time, and enhances employee experience.
2. Ensuring Data Privacy and Compliance
Employers must comply with HIPAA (Health Insurance Portability and Accountability Act) regulations to protect employee health data.
✔ Secure Online Platforms – Ensure encrypted communication between HR systems and insurance providers.
✔ Restricted Access – Limit access to sensitive health data to authorized HR personnel only.
✔ Compliance Audits – Conduct regular internal reviews to ensure adherence to HIPAA and ACA guidelines.
Failure to comply with data privacy laws can result in severe penalties and legal consequences.
3. Handling Claims and Disputes
Employers should establish a clear process for handling employee claims, disputes, and appeals.
✔ Educating Employees on Filing Claims – Employees should know how to submit claims, check status, and track reimbursements.
✔ Resolving Disputes – If an employee disagrees with a claim denial, HR should:
- Explain the reason for denial
- Guide them through the appeal process
- Provide direct contact information for insurance representatives
✔ Escalation Procedures – If an insurer wrongfully denies coverage, legal or regulatory escalation may be necessary.
By maintaining organized benefits administration, businesses can reduce confusion, minimize errors, and ensure employees receive the healthcare they need.
Maximizing Benefits and Cost Savings
Providing health insurance is a significant investment for businesses, but with the right strategies, wellness initiatives, and financial planning, employers can maximize benefits while reducing costs. By focusing on preventative care, leveraging tax advantages, and regularly reviewing insurance plans, businesses can ensure they provide high-quality, cost-effective healthcare solutions to employees.
Wellness Programs and Preventative Care
Investing in wellness programs and preventative healthcare leads to healthier employees, increased productivity, and long-term cost savings. Preventative care reduces the incidence of chronic illnesses, lowers medical expenses, and improves overall employee well-being.
1. Encouraging Healthy Lifestyles
Employers can promote a culture of health and wellness through workplace initiatives that encourage employees to make healthier lifestyle choices.
✔ On-Site or Virtual Wellness Programs – Offer fitness challenges, yoga sessions, or health coaching to motivate employees.
✔ Nutritional Support – Provide healthy snacks in the workplace, meal planning assistance, and dietitian consultations.
✔ Smoking Cessation Programs – Offer incentives for quitting smoking, such as reduced insurance premiums or reimbursement for smoking cessation products.
✔ Mental Health Support – Encourage the use of Employee Assistance Programs (EAPs), stress management workshops, and access to mental health professionals.
✔ Ergonomic Workstations – Invest in standing desks, proper seating, and ergonomic office setups to prevent workplace injuries.
A well-structured wellness program helps employees adopt healthier habits, leading to fewer medical claims and lower healthcare costs for employers.
2. Reducing Long-Term Healthcare Costs
Preventative care measures not only improve employee health but also reduce long-term insurance costs by preventing chronic conditions such as diabetes, heart disease, and hypertension.
✔ Annual Health Screenings – Encourage employees to undergo routine check-ups, blood pressure monitoring, and cholesterol screenings.
✔ Vaccination Programs – Provide flu shots, COVID-19 vaccines, and other preventive immunizations at no cost to employees.
✔ Chronic Disease Management – Offer support for diabetes, hypertension, and heart disease through telemedicine, health coaching, and medication assistance.
✔ Incentives for Preventative Care Participation – Reduce employee premiums or offer financial rewards for completing annual check-ups, physicals, or screenings.
Investing in preventative care leads to fewer sick days, lower absenteeism, and reduced insurance claims, ultimately saving businesses money while enhancing workforce well-being.
Tax Advantages of Employer-Sponsored Health Insurance
Businesses can significantly lower health insurance costs by taking advantage of tax deductions, credits, and specialized accounts.
1. Understanding Deductions and Credits
Employers can deduct the cost of health insurance premiums as a business expense, reducing taxable income.
✔ Employer Contributions Are Tax-Deductible – The amount a business contributes to employee premiums is fully tax-deductible.
✔ Small Business Health Care Tax Credit – Available for businesses with fewer than 25 employees, covering up to 50% of premium costs.
✔ Pre-Tax Contributions Lower Payroll Taxes – Employee contributions to Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs) are made pre-tax, reducing payroll tax liabilities.
✔ Self-Employed Health Insurance Deduction – Business owners can deduct 100% of health insurance premiums from self-employment income.
Employers should work with financial advisors or tax professionals to ensure they maximize available tax credits and deductions.
2. Health Reimbursement Arrangements (HRAs)
Health Reimbursement Arrangements (HRAs) are employer-funded accounts that allow businesses to reimburse employees for qualified medical expenses tax-free.
Types of HRAs:
✔ Qualified Small Employer HRA (QSEHRA) – Designed for businesses with fewer than 50 employees, allowing reimbursement for individual health plans and medical expenses.
✔ Individual Coverage HRA (ICHRA) – Provides employees with tax-free reimbursement for health insurance purchased on the private marketplace.
✔ Integrated HRA – Works alongside group health insurance to cover additional out-of-pocket costs such as deductibles and copayments.
HRAs help reduce costs for both employers and employees while offering greater flexibility in health plan selection.
3. Flexible Spending Accounts (FSAs)
A Flexible Spending Account (FSA) allows employees to set aside pre-tax dollars to pay for medical expenses, reducing their taxable income and saving money for employers.
✔ Covers out-of-pocket healthcare costs – Employees can use FSAs for copayments, deductibles, prescriptions, and some over-the-counter medications.
✔ Employer Tax Savings – Contributions to FSAs are not subject to payroll taxes, reducing employer tax liability.
✔ Annual Contribution Limits – Employees can contribute up to $3,200 (as of 2024) tax-free.
Employers can offer FSAs alongside health insurance plans to help employees manage medical costs efficiently.
Regular Plan Review and Adjustment
Health insurance plans should be monitored and adjusted periodically to ensure they remain cost-effective and meet employee needs.
1. Monitoring Employee Satisfaction and Utilization
To determine if a health plan is working, employers should gather feedback from employees and analyze healthcare usage data.
✔ Employee Surveys – Conduct annual benefits satisfaction surveys to assess how well the plan meets employee needs.
✔ Claims and Utilization Reports – Review insurance claims data to identify trends in healthcare usage and areas for cost reduction.
✔ HR Consultations – Work with HR teams to address employee concerns, coverage gaps, and plan efficiency.
✔ Adjust Coverage as Needed – Modify deductibles, copayments, and covered services based on feedback and financial considerations.
2. Adapting to Changing Healthcare Laws
Employers must stay informed about healthcare regulations to ensure compliance and take advantage of new incentives.
✔ Affordable Care Act (ACA) Updates – Stay up to date with new ACA mandates, affordability thresholds, and compliance changes.
✔ State-Specific Mandates – Some states have additional health insurance requirements beyond federal laws.
✔ Expanding Telemedicine & Digital Health Coverage – As telehealth services become more mainstream, businesses may need to update their benefits.
✔ New Tax Credits or Incentives – Regularly review government incentives that may reduce employer costs.
Staying ahead of regulatory changes ensures businesses remain compliant while optimizing benefits.
3. Negotiating with Insurers for Better Rates
Employers should regularly negotiate with insurance providers to secure better coverage at lower costs.
✔ Review Multiple Insurers – Compare different providers to find the most cost-effective plans.
✔ Leverage Employee Health Data – If claims are lower than expected, businesses can negotiate lower premium rates.
✔ Consider Self-Funded Plans – Larger companies may benefit from self-funding healthcare costs instead of traditional insurance.
✔ Utilize Insurance Brokers – Work with brokers to identify cost-saving strategies and alternative plan options.
By optimizing insurance negotiations, businesses can reduce expenses without compromising employee health benefits.
Key Takeaways for Employers
✔ Investing in wellness programs and preventative care reduces healthcare costs while improving employee well-being.
✔ Utilizing tax benefits like HRAs, FSAs, and small business tax credits can significantly lower insurance expenses.
✔ Regularly reviewing and adjusting plans ensures coverage remains cost-effective and meets employee needs.
✔ Employers must stay informed about healthcare laws and negotiate with insurers for better rates.
















Content that may interest you