
Corporate medical insurance for employees
In today's competitive business environment, offering comprehensive medical insurance is essential for attracting and retaining top talent. Corporate medical insurance provides employees with access to healthcare services, promoting their well-being and enhancing productivity. This article explores the various aspects of corporate medical insurance, helping employers understand its importance and how to implement effective health benefits.
Corporate medical insurance, also known as group health insurance, is a policy purchased by employers to provide healthcare coverage to their employees. This coverage typically includes medical expenses such as doctor visits, hospital stays, surgeries, and prescription drugs. Offering such benefits not only safeguards employees' health but also contributes to job satisfaction and loyalty.
Benefits of Providing Health Insurance to Employees
Offering health insurance as part of an employee benefits package is no longer just an option—it is a strategic business decision that directly impacts employee satisfaction, business performance, and financial stability. Health benefits help attract and retain top talent, reduce tax liabilities, and improve workforce productivity, making them an essential investment for any organization.
This guide explores the key advantages of providing health insurance to employees, highlighting how it benefits both employers and employees alike.
1. Attracting and Retaining Top Talent
Why Health Benefits Matter for Recruitment and Retention
In a competitive job market, offering health insurance can set your company apart from others that do not provide comprehensive benefits. Employees prioritize healthcare coverage when choosing an employer, and businesses with strong health benefits have an advantage in attracting high-quality professionals.
How Health Insurance Attracts Talent
✔ Competitive Hiring Advantage:
- Job seekers prioritize companies that offer comprehensive health coverage.
- Businesses that provide medical benefits have higher applicant interest and better hiring success rates.
✔ Enhanced Employer Branding:
- Companies known for great employee benefits attract top-tier professionals.
- Strong employer branding improves word-of-mouth recommendations and job satisfaction rates.
✔ Appealing to a Diverse Workforce:
- Younger employees value preventive care, wellness programs, and mental health support.
- Older employees prioritize chronic disease management, prescription drug coverage, and family benefits.
How Health Insurance Improves Retention
✔ Lower Employee Turnover:
- Employees with comprehensive health benefits are more likely to stay with their employer.
- Retaining employees reduces recruitment and training costs, saving businesses thousands of dollars annually.
✔ Stronger Employee Loyalty:
- Workers who feel valued and supported through health benefits are more loyal and engaged.
- Businesses that invest in employee well-being see higher job satisfaction levels.
✔ Why It Matters?
Providing health insurance enhances employee retention, reduces turnover costs, and makes a company more attractive to skilled professionals.
2. Tax Advantages for Employers
How Business Health Insurance Reduces Tax Burdens
Employers who offer group health insurance can benefit from significant tax incentives, including credits, deductions, and payroll tax savings.
Key Tax Benefits for Employers
✔ Small Business Health Care Tax Credit:
- Businesses with fewer than 25 full-time employees may qualify for a tax credit of up to 50% of premium costs.
- To be eligible, employers must:
- Offer coverage through the Small Business Health Options Program (SHOP).
- Cover at least 50% of employee premiums.
- Have an average employee salary of $58,000 or less per year (subject to adjustments).
✔ Tax Deductibility of Premiums:
- Employer-paid premiums are tax-deductible business expenses, reducing taxable income.
- This helps offset the costs of offering comprehensive benefits.
✔ Payroll Tax Savings:
- Employer contributions toward employee health insurance are not subject to payroll taxes.
- Employees can pay their share of premiums using pre-tax dollars, reducing their taxable income.
✔ Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs):
- Employers contributing to HSAs and FSAs provide employees with pre-tax savings for medical expenses.
- HSA contributions by employers are also tax-deductible.
✔ Why It Matters?
Offering health benefits reduces tax liabilities for businesses, saving money while improving employee satisfaction.
3. Enhanced Employee Productivity and Reduced Absenteeism
How Health Insurance Improves Workforce Performance
Providing health insurance directly impacts employee health, morale, and productivity, leading to a more efficient and engaged workforce.
Key Productivity Benefits of Offering Health Insurance
✔ Access to Preventive Care and Early Treatment:
- Employees with regular access to healthcare are more likely to undergo preventive check-ups, reducing the risk of chronic illnesses.
- Early diagnosis and treatment prevent long-term medical complications, keeping employees healthier.
✔ Lower Absenteeism and Sick Leave:
- Workers with comprehensive health coverage take fewer sick days.
- Proper medical care helps employees recover faster, leading to higher attendance and productivity.
✔ Mental Health and Stress Reduction:
- Many business health plans include mental health coverage, helping employees manage stress, anxiety, and burnout.
- Employees with access to mental health services are more focused, engaged, and productive.
✔ Higher Workplace Morale and Job Satisfaction:
- When employees feel supported in their health and well-being, their motivation and commitment to their job increases.
- Businesses that invest in health benefits foster a culture of loyalty and appreciation.
✔ Workplace Safety & Chronic Disease Management:
- Health insurance plans often include disease management programs that help employees manage chronic conditions effectively.
- Reducing workplace injuries and long-term medical issues leads to lower compensation claims and legal risks.
✔ Why It Matters?
Providing business medical insurance enhances employee well-being, reduces absenteeism, and leads to a more productive workforce, directly benefiting company performance.
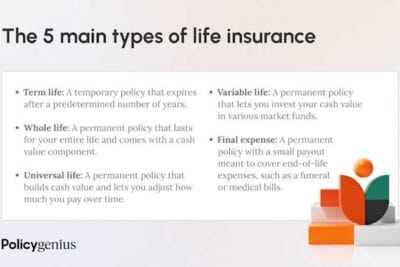
Types of Corporate Health Insurance Plans
Selecting the right corporate health insurance plan is a crucial decision for businesses, as it directly impacts employee well-being, financial sustainability, and overall business performance. Employers must consider factors such as costs, coverage flexibility, and network access when choosing a plan that aligns with their company’s needs.
This guide provides a detailed breakdown of the most common types of corporate health insurance plans, including traditional group insurance, Health Reimbursement Arrangements (HRAs), and self-funded health plans. Understanding these options will help businesses make informed decisions to offer the best possible healthcare benefits to employees.
1. Traditional Group Health Insurance Plans
What Are Traditional Group Health Insurance Plans?
Traditional group health insurance is the most common form of employer-sponsored healthcare coverage. Under these plans, businesses purchase policies from an insurance provider, and both employers and employees share the premium costs.
Key Features of Traditional Group Health Plans:
✔ Employer-Employee Cost Sharing: Employers pay a portion of the premiums, while employees contribute through payroll deductions.
✔ Comprehensive Medical Coverage: Includes doctor visits, hospital stays, prescription medications, and preventive care.
✔ Pre-Negotiated Provider Networks: Employees receive discounted rates when using in-network healthcare providers.
✔ Regulatory Compliance: These plans typically meet Affordable Care Act (ACA) requirements, avoiding penalties.
Types of Traditional Group Health Plans:
1.1 Health Maintenance Organizations (HMOs)
HMO plans are structured to provide lower-cost healthcare options but require employees to use a network of designated providers.
Key Characteristics of HMOs:
✔ Primary Care Physician (PCP) Requirement:
- Employees must select a PCP who serves as the first point of contact for healthcare services.
- Referrals from the PCP are required for specialist visits.
✔ Strict Network Limitations:
- Employees must use in-network providers for coverage to apply (except in emergencies).
- Out-of-network services are generally not covered.
✔ Lower Premiums and Out-of-Pocket Costs:
- HMOs tend to have lower premiums, deductibles, and copays.
- Many preventive care services are covered at no cost.
✔ Why Choose an HMO?
- Best for businesses looking for cost-effective coverage with predictable expenses.
- Ideal for employees who prefer a structured network with coordinated care.
1.2 Preferred Provider Organizations (PPOs)
PPO plans offer greater flexibility than HMOs by allowing employees to visit any healthcare provider without requiring referrals.
Key Characteristics of PPOs:
✔ No Referral Needed for Specialists:
- Employees can see any doctor or specialist without PCP approval.
- More autonomy in choosing healthcare providers.
✔ In-Network vs. Out-of-Network Coverage:
- Employees receive lower costs for in-network providers.
- Out-of-network care is covered, but at a higher cost.
✔ Higher Premiums but More Flexibility:
- PPOs typically have higher monthly premiums than HMOs.
- Employees have access to a broader selection of doctors and hospitals.
✔ Why Choose a PPO?
- Suitable for businesses with employees who need specialist access or frequently travel.
- Ideal for companies that want to offer flexibility in provider choices.
1.3 Exclusive Provider Organizations (EPOs)
EPO plans combine elements of HMOs and PPOs, offering a balance between cost savings and flexibility.
Key Characteristics of EPOs:
✔ No PCP or Referral Requirements:
- Employees can visit specialists directly without requiring a referral.
✔ Strict Network Limitations:
- Employees must use in-network providers only, except in emergencies.
- No coverage for out-of-network services.
✔ Moderate Costs & Balanced Coverage:
- Typically lower premiums than PPOs but higher than HMOs.
- Employees still benefit from cost savings within the provider network.
✔ Why Choose an EPO?
- Best for businesses looking for a cost-effective plan with some flexibility.
- Suitable for employees who do not require out-of-network care but want direct specialist access.
2. Health Reimbursement Arrangements (HRAs)
What Is an HRA?
A Health Reimbursement Arrangement (HRA) is an employer-funded health benefit that reimburses employees for qualified medical expenses. Unlike traditional insurance plans, HRAs allow businesses to set a pre-defined reimbursement limit rather than paying fixed premiums to an insurance provider.
Key Features of HRAs:
✔ Employer-Controlled Contributions:
- Employers determine the maximum amount available for reimbursement.
- Employees are reimbursed tax-free for eligible healthcare costs.
✔ Flexible Plan Structures:
- HRAs can be used to cover insurance premiums, copayments, deductibles, and medical expenses.
- Can be paired with high-deductible health plans (HDHPs) to control costs.
✔ Unused Funds May Roll Over:
- Depending on plan design, unused balances may be carried over year to year.
✔ Why Choose an HRA?
- Ideal for small businesses seeking cost-effective, flexible health benefits.
- Offers greater control over healthcare spending while allowing employees to choose individual insurance plans.
3. Self-Funded Health Plans
What Is a Self-Funded Health Plan?
A self-funded (self-insured) health plan is an alternative to traditional insurance where the employer assumes financial responsibility for employee healthcare claims rather than paying fixed premiums to an insurer.
How Self-Funded Plans Work:
✔ Employer Pays for Claims Directly:
- Instead of paying an insurance company, the employer covers medical claims as they arise.
- Reduces administrative costs and allows customization of benefits.
✔ Third-Party Administrators (TPAs) Handle Claims:
- Employers partner with TPAs to process claims, manage provider networks, and handle compliance.
✔ Stop-Loss Insurance for Risk Protection:
- Employers purchase stop-loss insurance to limit exposure to catastrophic healthcare claims.
✔ Cost Efficiency & Customization:
- Businesses only pay for actual claims, avoiding inflated insurance premiums.
- Employers can design custom health benefits based on employee needs.
✔ Why Choose a Self-Funded Plan?
- Best for large businesses with a stable workforce that can manage fluctuating healthcare costs.
- Suitable for companies looking to gain control over healthcare expenses while customizing benefits.
Legal Requirements for Employers
Employers offering corporate health insurance must comply with various federal and state regulations to ensure their plans meet minimum standards for coverage, affordability, and accessibility. Failure to adhere to these regulations can result in financial penalties, legal issues, and employee dissatisfaction.
This guide outlines the key legal requirements employers must follow when offering health insurance, focusing on Affordable Care Act (ACA) compliance and state-specific mandates.
1. Affordable Care Act (ACA) Compliance
The Affordable Care Act (ACA), enacted in 2010, established comprehensive reforms to expand healthcare access and improve insurance affordability. It imposes specific employer mandates, primarily affecting companies with 50 or more full-time employees (FTEs).
1.1 Employer Shared Responsibility Requirements
Employers classified as Applicable Large Employers (ALEs)—those with 50 or more FTEs—are subject to the Employer Shared Responsibility (ESR) provisions under the ACA.
Key ACA Compliance Requirements for Employers:
✔ Minimum Essential Coverage (MEC):
- Employers must offer qualifying health insurance plans that include preventive care, hospitalization, mental health services, and prescription drug coverage.
- Plans must comply with the Minimum Value Standard (MVS), meaning they must cover at least 60% of the total cost of healthcare expenses.
✔ Affordability Standard:
- The employee’s share of the premium for self-only coverage cannot exceed 9.12% of their household income (as of 2023, subject to annual adjustments).
- Employers must ensure that low-income employees can afford their contributions.
✔ Coverage for Full-Time Employees & Dependents:
- Employers must offer coverage to at least 95% of full-time employees (defined as those working 30+ hours per week).
- Coverage must extend to dependents up to age 26, but not necessarily to spouses.
✔ Prohibition on Discriminatory Practices:
- Employers cannot favor highly compensated employees in their health plan offerings.
- Plans must be equally accessible to all eligible workers.
1.2 ACA Reporting Requirements
Employers subject to ACA regulations must file specific forms with the IRS to document compliance.
✔ Form 1095-C:
- Reports whether an employer offered coverage to full-time employees.
- Must be provided to both employees and the IRS.
✔ Form 1094-C:
- Serves as a transmittal document summarizing employer-provided health coverage.
✔ W-2 Reporting:
- Employers must report the total cost of employer-sponsored health coverage to employees.
✔ Why It Matters?
Employers who fail to offer qualifying coverage or comply with reporting requirements may face substantial penalties from the IRS.
1.3 ACA Penalties for Non-Compliance
The ACA imposes two primary financial penalties for employers who fail to comply with health insurance mandates.
1. Failure to Offer Minimum Essential Coverage (Penalty A – “Sledgehammer Penalty”)
- Applies when an employer does not offer health insurance to at least 95% of full-time employees.
- Penalty: $2,970 per full-time employee (excluding the first 30 employees).
2. Offering Non-Compliant or Unaffordable Coverage (Penalty B – “Tackhammer Penalty”)
- Applies when an employer offers coverage that does not meet affordability or minimum value standards.
- Penalty: $4,460 per affected employee who receives subsidized coverage through the ACA marketplace.
✔ Why It Matters?
Non-compliance with ACA regulations can lead to significant financial penalties and reputational damage, making it critical for businesses to monitor their coverage offerings carefully.
2. State-Specific Health Insurance Mandates
While the ACA establishes federal guidelines, some states impose additional mandates requiring employers to provide expanded benefits, minimum employer contributions, or additional reporting.
2.1 Common State-Specific Employer Requirements
✔ Employer Contribution Requirements:
- Some states require employers to pay a minimum percentage of employee premiums to ensure affordability.
- Example:
- Hawaii Prepaid Health Care Act: Employers must cover at least 50% of employee health insurance premiums for employees working 20+ hours per week.
✔ State-Based Individual Mandates & Employer Reporting:
- Some states require individuals to have health insurance and mandate employer reporting to ensure compliance.
- Examples of States with Individual Mandates:
- California, New Jersey, Rhode Island, and Massachusetts require employers to report health coverage information to state tax agencies.
- Washington, D.C., and Vermont impose penalties on residents who do not have adequate health coverage.
✔ Mandated Benefits Beyond ACA Standards:
- Some states require expanded health benefits that go beyond federal ACA minimums.
- Examples of Additional State-Mandated Benefits:
- Infertility treatment coverage (e.g., New York, Massachusetts, Illinois).
- Expanded mental health and substance abuse treatment (e.g., Oregon, Connecticut).
- Paid family and medical leave programs (e.g., California, New York, Washington).
✔ State-Specific Small Business Health Insurance Programs:
- Some states offer subsidized small business health plans with additional employer requirements.
- Example:
- California’s Covered California for Small Business (CCSB) provides ACA-compliant group health plans for small employers.
✔ Why It Matters?
Employers with multi-state operations must stay informed on local requirements to ensure full compliance and avoid penalties.
Steps to Obtain a Business Medical Insurance Quote
Securing a business medical insurance quote is an essential step for companies looking to provide quality healthcare benefits to employees. The right health insurance plan ensures comprehensive coverage, enhances employee satisfaction, and helps businesses stay competitive while managing costs.
This guide outlines the step-by-step process for obtaining a business health insurance quote, ensuring that employers make informed and strategic decisions.
1. Assess Your Business Needs
Before requesting quotes, employers must evaluate their workforce needs, financial constraints, and compliance obligations. This step helps businesses choose a health plan that aligns with employee expectations while remaining cost-effective.
Key Factors to Consider:
✔ Employee Demographics:
- Analyze the age distribution, health conditions, and family status of employees.
- Younger employees may prioritize preventive care and mental health services, while older employees may require specialist access and chronic disease management.
- Determine whether employees need individual or family coverage.
✔ Budget Constraints:
- Determine how much the company can afford to contribute toward health insurance premiums.
- Evaluate the cost-sharing structure between employer and employees.
- Factor in additional costs, such as deductibles, copayments, and out-of-pocket maximums.
✔ Regulatory Compliance Requirements:
- Businesses with 50+ full-time employees (FTEs) must comply with Affordable Care Act (ACA) mandates.
- Multi-state businesses must check state-specific health insurance requirements.
✔ Why It Matters?
A well-defined budget and workforce analysis ensures that the selected health plan meets both employer financial goals and employee healthcare needs.
2. Research Potential Insurance Providers
Choosing a reliable health insurance provider is critical to securing competitive rates, quality service, and comprehensive coverage. Employers should compare several insurers before making a final decision.
How to Evaluate Insurance Providers:
✔ Reputation and Financial Stability:
- Choose insurers with high financial ratings and strong industry reviews.
- Verify ratings from AM Best, Moody’s, or Standard & Poor’s.
- Research customer satisfaction and claim processing speed.
✔ Plan Options and Flexibility:
- Ensure the provider offers multiple plan types (e.g., HMO, PPO, HDHP, EPO).
- Look for customizable coverage options, including dental, vision, mental health, and wellness programs.
✔ Network Size and Accessibility:
- Evaluate the provider’s network of hospitals, physicians, and specialists.
- Ensure employees have access to in-network providers near their locations.
- Check if telemedicine services are included for remote and flexible care options.
✔ Customer Support and Digital Tools:
- Look for 24/7 customer service support for claims and benefits inquiries.
- Ensure the provider offers digital tools, such as online portals and mobile apps, for easy benefits management.
✔ Why It Matters?
Selecting a trustworthy and financially stable provider ensures long-term cost savings, reliable claims processing, and improved employee satisfaction.
3. Gather Necessary Information
To receive an accurate insurance quote, businesses must provide insurers with detailed company and employee data.
Essential Data to Collect:
✔ Employee Census Data:
- Number of full-time and part-time employees.
- Employee demographics (age, gender, dependent status).
- Average salary levels (if applicable for plan eligibility).
✔ Current Benefits Package (if applicable):
- Review existing coverage and cost structure.
- Identify gaps in coverage and areas for improvement.
- Compare whether new plans offer better value.
✔ Employer Contribution Plan:
- Determine how much the employer currently contributes or plans to contribute to premiums.
- Decide if employees will have access to voluntary benefits such as HSAs or FSAs.
✔ Why It Matters?
Providing accurate data ensures that quotes reflect realistic pricing and plan offerings, avoiding unexpected cost discrepancies.
4. Request Quotes from Multiple Providers
To secure the best pricing and coverage, employers should request multiple quotes from different providers.
How to Obtain and Compare Quotes:
✔ Contact Multiple Insurance Providers:
- Request quotes from both national and regional insurers to compare rates.
- Consider fully insured vs. self-funded plan options if applicable.
✔ Utilize Brokers or Agents:
- Insurance brokers help negotiate better pricing and provide expert plan recommendations.
- Brokers can simplify the paperwork and compliance process.
✔ Industry and Trade Associations:
- Some industry groups offer health insurance discounts for member businesses.
✔ Why It Matters?
Comparing multiple quotes ensures cost-effectiveness and better plan customization, helping businesses make an informed choice.
5. Compare and Analyze Quotes
Once quotes are obtained, employers must carefully compare the details to determine the best plan.
Key Factors to Compare:
✔ Coverage Details:
- Verify included services like preventive care, hospitalization, prescription drugs, and mental health support.
- Look for wellness incentives and telehealth options.
✔ Cost-Sharing Structure:
- Compare premiums, deductibles, copayments, and out-of-pocket maximums.
- Evaluate employer contribution percentages and potential employee financial burdens.
✔ Provider Networks:
- Confirm whether preferred doctors, hospitals, and specialists are included in the network.
- Ensure that out-of-network coverage is available if needed.
✔ Plan Add-Ons & Extra Benefits:
- Consider dental, vision, mental health, and alternative medicine options.
- Look for employee wellness incentives (e.g., gym memberships, health coaching).
✔ Why It Matters?
A thorough analysis prevents hidden costs, ensures comprehensive coverage, and improves employee satisfaction with the selected plan.
6. Make an Informed Decision
Before finalizing a business medical insurance plan, employers should consider long-term impact and employee preferences.
Key Decision-Making Factors:
✔ Employee Input & Feedback:
- Conduct employee surveys to gauge preferences and identify must-have benefits.
- Host Q&A sessions to educate employees on their options.
✔ Long-Term Business Growth & Scalability:
- Ensure the plan can accommodate company growth and changing workforce demographics.
- Evaluate whether renewal pricing and benefits adjustments will be manageable.
✔ Regulatory and Compliance Review:
- Ensure the plan meets ACA and state-specific requirements to avoid penalties.
✔ Why It Matters?
Making an informed, strategic decision ensures the selected health plan aligns with both financial and employee wellness goals.
Common Challenges and Solutions
Providing business health insurance is essential for maintaining a healthy and productive workforce, but it comes with several challenges. Employers must balance rising healthcare costs, manage administrative complexities, and stay compliant with evolving regulations.
This guide explores the most common obstacles businesses face when offering health insurance and provides practical solutions to overcome them.
1. Rising Premium Costs
The Challenge: Increasing Healthcare Expenses
One of the most pressing concerns for employers is the continuous rise in health insurance premiums. Factors such as medical inflation, increased chronic diseases, and high-cost treatments contribute to escalating healthcare expenses.
Key Factors Driving Higher Premiums:
✔ Medical Inflation: Healthcare costs—including hospital stays, surgeries, and specialist visits—are rising annually.
✔ Chronic Health Conditions: More employees suffer from diabetes, hypertension, and obesity, leading to higher healthcare utilization.
✔ Expensive Prescription Drugs: The increasing costs of brand-name and specialty medications drive up insurance premiums.
✔ Aging Workforce: Older employees require more frequent medical care, increasing insurance claims and costs.
Solutions to Control Rising Premium Costs:
1. Implement Wellness Programs
Encouraging healthy habits and preventive care can significantly reduce healthcare costs by minimizing the need for expensive treatments.
✔ Preventive Health Screenings & Vaccinations:
- Offer free or subsidized annual check-ups, flu shots, and biometric screenings to detect health issues early.
✔ Fitness & Physical Activity Programs:
- Provide discounted gym memberships, step-count challenges, and wellness incentives to encourage an active lifestyle.
✔ Mental Health Support:
- Include Employee Assistance Programs (EAPs), stress management resources, and telehealth counseling services.
✔ Smoking Cessation & Nutritional Counseling:
- Offer financial incentives for employees to quit smoking or adopt healthier eating habits.
2. Explore Different Plan Structures
Revising the structure of health plans can help lower costs while maintaining adequate coverage.
✔ High-Deductible Health Plans (HDHPs) with Health Savings Accounts (HSAs):
- Lower monthly premiums in exchange for higher deductibles.
- Employees can save pre-tax dollars in HSAs for medical expenses.
✔ Tiered Network Plans:
- Offer lower-cost providers within a preferred network, reducing out-of-pocket expenses for employees.
✔ Self-Funded or Partially-Funded Plans:
- Employers with predictable healthcare costs can opt for self-insurance, covering claims directly instead of paying fixed premiums.
✔ Why It Matters?
By proactively managing healthcare costs, businesses can offer competitive benefits without compromising financial sustainability.
2. Administrative Burden
The Challenge: Managing Complex Health Insurance Processes
Administering business health insurance involves significant paperwork, compliance tracking, and ongoing management. HR teams often face challenges in managing enrollments, processing claims, and handling employee inquiries.
Common Administrative Challenges:
✔ Plan Selection & Renewal: HR teams must review multiple plan options, costs, and benefits annually.
✔ Employee Enrollment & Support: Employees often struggle to understand their benefits, leading to frequent HR inquiries.
✔ Regulatory Compliance & Claims Processing: Businesses must ensure accurate reporting, adherence to federal/state laws, and timely claims resolution.
Solutions to Reduce Administrative Complexity:
1. Utilize Technology to Streamline Benefits Management
Adopting HR and benefits management software can automate and simplify health insurance administration.
✔ Cloud-Based Benefits Platforms:
- Employees can self-enroll, track claims, and compare plan options through an online portal.
- Reduces paperwork and improves data accuracy.
✔ Payroll & Benefits Integration:
- Automates payroll deductions and employer contributions for health insurance.
✔ AI-Powered Employee Support Tools:
- Chatbots and automated systems can handle frequently asked employee questions about health benefits.
2. Outsource Benefits Administration
For companies with limited HR resources, outsourcing benefits management can reduce errors and administrative workload.
✔ Third-Party Administrators (TPAs):
- Handle claims processing, benefits enrollment, and regulatory compliance on behalf of employers.
✔ Insurance Brokers & Benefits Consultants:
- Provide expert guidance on plan selection, negotiations, and employee benefits education.
✔ Why It Matters?
By leveraging technology and outsourcing services, businesses can reduce administrative complexity, minimize errors, and improve employee benefits experience.
3. Keeping Up with Regulatory Changes
The Challenge: Constantly Evolving Healthcare Laws
Health insurance regulations frequently change, requiring businesses to stay updated to maintain compliance. Failure to adhere to federal or state mandates can result in substantial penalties and legal consequences.
Key Compliance Requirements Employers Must Manage:
✔ Affordable Care Act (ACA) Requirements:
- Employers with 50+ full-time employees must provide affordable, minimum essential coverage (MEC).
- Failure to comply results in Employer Shared Responsibility (ESR) penalties.
✔ State-Specific Health Insurance Mandates:
- Some states impose additional reporting obligations and coverage standards beyond federal laws.
✔ HIPAA Compliance & Data Security:
- Employers handling employee health information must follow Health Insurance Portability and Accountability Act (HIPAA) guidelines.
✔ COBRA Administration:
- Companies with 20+ employees must provide continuation coverage options for terminated employees.
- Failure to manage COBRA notices correctly can lead to federal fines.
Solutions to Stay Compliant with Health Insurance Laws:
1. Invest in Ongoing Compliance Training for HR Teams
✔ Attend Healthcare Compliance Workshops & Seminars:
- Stay updated on legislative changes, IRS reporting requirements, and state health laws.
✔ Internal Compliance Audits:
- Regularly review benefits policies to ensure full legal compliance.
2. Consult Legal and Compliance Experts
✔ Work with Healthcare Law Attorneys:
- Provide expert advice on navigating regulatory changes.
- Assist with risk management and compliance strategies.
✔ Hire HR Compliance Specialists:
- Ensure ACA reporting, HIPAA privacy, and COBRA administration are properly handled.
✔ Why It Matters?
By staying informed and partnering with compliance professionals, employers can avoid regulatory penalties and ensure their health benefits align with legal requirements.
















Content that may interest you