
Business health insurance
Providing health insurance is a critical aspect of running a successful business, as it not only ensures the well-being of employees but also enhances job satisfaction and retention. Understanding the various facets of business health insurance can help employers make informed decisions that align with both company objectives and employee needs.
I. Introduction to Business Health Insurance
Business health insurance is a crucial component of a comprehensive employee benefits package. It provides coverage for medical expenses, helping employees access essential healthcare services while reducing financial burdens. For employers, offering health insurance is not just about compliance with regulations—it is also a strategic investment that enhances workforce well-being, boosts productivity, and strengthens employee retention.
A. Definition and Importance
What is Business Health Insurance?
Business health insurance, also known as group health insurance, is a policy that employers offer to their employees to cover medical expenses. It typically includes coverage for:
- Doctor visits
- Hospital stays and emergency care
- Preventive services (vaccinations, screenings, annual check-ups)
- Prescription drugs
- Mental health services
- Specialist consultations
- Dental and vision care (optional add-ons)
These plans are often more affordable than individual health plans because the risk is spread across multiple employees, leading to lower premiums.
Why is Business Health Insurance Important?
Providing health insurance is not just a legal requirement for some businesses—it also delivers significant advantages to both employers and employees.
1. Attracting and Retaining Talent
- Employees consider health benefits one of the most important factors when choosing a job.
- Businesses that offer comprehensive health coverage gain a competitive edge in recruitment.
2. Boosting Employee Productivity
- Healthy employees take fewer sick days, reducing absenteeism.
- Access to preventive care helps employees manage chronic conditions before they become severe.
- Mental health support improves focus, reducing workplace stress and burnout.
3. Improving Employee Satisfaction and Loyalty
- A robust benefits package leads to higher job satisfaction and morale.
- Employees with health insurance feel more valued and secure, leading to better engagement and performance.
4. Tax Benefits for Employers
- Employers can deduct health insurance premiums as a business expense.
- Companies that qualify for the Small Business Health Care Tax Credit can offset costs by up to 50%.
B. Legal Requirements
Health insurance requirements vary based on business size, location, and industry. Understanding these obligations helps businesses remain compliant and avoid financial penalties.
1. Affordable Care Act (ACA) Mandate
The Affordable Care Act (ACA) imposes specific regulations on employers regarding health insurance:
Employer Mandate for Large Businesses (50+ Employees)
- Businesses with 50 or more full-time employees (or full-time equivalent employees) must provide affordable health insurance that meets minimum essential coverage (MEC).
- Coverage must be affordable, meaning the employee’s share of the premium cannot exceed 9.12% of their household income (as of 2023).
- Failing to offer health insurance can result in significant penalties under the Employer Shared Responsibility Payment (ESRP).
Small Businesses (Fewer than 50 Employees)
- Businesses with fewer than 50 employees are not legally required to offer health insurance.
- However, they may qualify for the Small Business Health Options Program (SHOP), which provides tax credits to offset premium costs.
| Business Size | Health Insurance Requirement | Potential Penalty |
| 1-49 Employees | Not required, but eligible for SHOP tax credits. | No penalty for not offering coverage. |
| 50+ Employees | Must provide affordable, ACA-compliant coverage. | $2,970 per employee (if no coverage is provided). |
2. COBRA (Consolidated Omnibus Budget Reconciliation Act)
- Employers with 20+ employees must offer continuation coverage for employees who leave the company.
- COBRA allows employees to keep their employer-sponsored health insurance for 18 to 36 months, but they must pay the full premium cost.
3. ERISA (Employee Retirement Income Security Act)
- ERISA requires employers who offer health plans to provide transparent information about benefits, costs, and employee rights.
- Employers must follow non-discrimination rules, ensuring that health benefits are not structured to favor executives over other employees.
4. HIPAA (Health Insurance Portability and Accountability Act)
- Protects employee health information privacy.
- Ensures continuous coverage for employees switching jobs, preventing pre-existing condition exclusions in employer-sponsored plans.
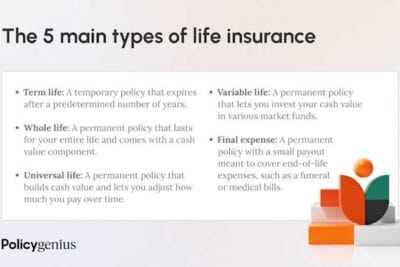
II. Types of Business Health Insurance Plans
Selecting the right business health insurance plan is a crucial decision for employers, as it affects both company finances and employee well-being. There are three main types of health insurance plans that businesses typically consider: fully insured plans, self-funded plans, and level-funded plans. Each type has its own structure, benefits, and risks, which employers must carefully evaluate based on their financial capacity and workforce needs.
A. Fully Insured Plans
What is a Fully Insured Plan?
A fully insured plan is the most traditional type of business health insurance. In this model, the employer pays a fixed premium to an insurance carrier, which assumes the financial risk of covering employees' healthcare costs.
The insurance carrier:
- Sets the premium rates based on factors such as company size, employee demographics, and past claims history.
- Manages all administrative tasks, including claims processing and compliance with healthcare regulations.
- Absorbs the financial risk, meaning that even if employees generate high medical costs, the employer is not responsible for additional expenses beyond the premium.
Pros of Fully Insured Plans
✔ Predictable Costs – Employers pay a fixed monthly premium, making budgeting and financial planning easier.
✔ Simplicity in Management – The insurance carrier handles claims processing, legal compliance, and provider networks, reducing the employer’s administrative burden.
✔ Lower Financial Risk – Since the insurance company assumes the risk, the employer is protected from unexpected high medical claims.
Cons of Fully Insured Plans
✖ Less Flexibility – Employers have limited ability to customize plan benefits, provider networks, and cost structures.
✖ Potentially Higher Long-Term Costs – Insurance carriers build profit margins into their premiums, which can lead to higher costs over time compared to self-funded alternatives.
✖ Annual Premium Increases – Insurance companies often raise premiums each year, making long-term budgeting challenging for businesses.
B. Self-Funded Plans
What is a Self-Funded Plan?
In a self-funded (or self-insured) plan, the employer assumes full financial responsibility for employee healthcare costs instead of paying fixed premiums to an insurance carrier.
Under this model:
- The employer pays for healthcare claims out-of-pocket as they arise, instead of a set monthly premium.
- A third-party administrator (TPA) typically manages claims processing, provider networks, and compliance.
- Employers often purchase stop-loss insurance to protect against unexpectedly high claims, limiting their financial risk.
Pros of Self-Funded Plans
✔ Greater Control Over Plan Design – Employers can customize coverage options, provider networks, and wellness programs to better suit their workforce.
✔ Potential Cost Savings – Businesses avoid insurance carrier profit margins and can save money if employees generate fewer claims.
✔ Cash Flow Benefits – Instead of prepaying for healthcare costs via premiums, employers only pay for actual claims incurred.
✔ No State-Mandated Premium Taxes – Self-funded plans are regulated under federal ERISA laws, exempting them from state insurance mandates and taxes.
Cons of Self-Funded Plans
✖ Financial Risk – If employees incur high medical costs, the employer bears the financial burden. Unexpected claims can impact cash flow and business stability.
✖ Regulatory Complexities – Employers must ensure compliance with federal laws such as ERISA, HIPAA, and ACA, which can be administratively challenging.
✖ Administrative Burden – Requires businesses to manage claims, provider contracts, and compliance unless outsourced to a TPA.
✖ Not Ideal for Small Businesses – Smaller companies with fewer employees may struggle with cash flow volatility caused by unpredictable healthcare claims.
C. Level-Funded Plans
What is a Level-Funded Plan?
A level-funded plan is a hybrid approach that combines aspects of fully insured and self-funded plans. It provides businesses with predictable costs while offering potential refunds if claims are lower than expected.
In a level-funded plan:
- The employer pays a fixed monthly amount to an insurance provider, similar to a fully insured plan.
- This amount covers anticipated healthcare claims, administrative fees, and stop-loss insurance.
- At the end of the year, if employee healthcare claims are lower than expected, the employer receives a refund or credit.
- If claims exceed expected costs, stop-loss insurance covers the overage.
Pros of Level-Funded Plans
✔ Predictable Costs – Like fully insured plans, businesses pay a fixed monthly amount, making budgeting easier.
✔ Potential Refunds – If claims are lower than projected, the employer may receive money back, reducing overall costs.
✔ Lower Risk Compared to Self-Funded Plans – Stop-loss insurance protects the employer from catastrophic claims, limiting financial exposure.
✔ Exempt from Certain State Insurance Taxes – Since level-funded plans are partially self-funded, they may be exempt from some state-mandated insurance taxes.
Cons of Level-Funded Plans
✖ Limited Plan Customization – While level-funded plans offer some flexibility, they still rely on insurance carrier guidelines.
✖ Possible Financial Risk – If healthcare claims exceed expectations, employers may face increased costs when renewing the plan.
✖ Not Always Available to Small Businesses – Some insurance carriers only offer level-funded plans to companies with a minimum number of employees (e.g., 10+).
Comparison Table: Fully Insured vs. Self-Funded vs. Level-Funded Plans
| Feature | Fully Insured Plan | Self-Funded Plan | Level-Funded Plan |
| Cost Predictability | High – Fixed premiums | Low – Costs vary based on claims | Medium – Fixed monthly payments with refund potential |
| Financial Risk | Low – Insurance company assumes risk | High – Employer assumes all risk | Medium – Stop-loss insurance limits major risks |
| Plan Customization | Low – Limited flexibility | High – Employer designs the plan | Medium – Some customization available |
| Administrative Burden | Low – Insurance provider handles claims and compliance | High – Employer must manage or hire a TPA | Medium – Insurance provider manages some administrative tasks |
| Potential Cost Savings | Low – Premiums include insurer’s profit margin | High – No insurance carrier profit margin | Medium – Possible refund if claims are low |
| Regulatory Compliance | Must follow state and federal laws | Regulated under federal ERISA laws | Typically follows ERISA guidelines but varies by provider |
III. Factors to Consider When Choosing a Plan
Selecting the right business health insurance plan requires careful evaluation of various factors to ensure that it meets the financial, medical, and accessibility needs of both employers and employees. A well-structured health plan not only provides comprehensive medical coverage but also helps businesses control costs and improve employee satisfaction. Below are the key factors that businesses should consider when choosing the best health insurance plan for their workforce.
A. Employee Demographics
Understanding employee demographics is essential for tailoring a health insurance plan that effectively meets the needs of the workforce. The following factors should be carefully analyzed:
1. Age Distribution
- Younger employees (20s–30s) may prioritize lower premiums and high-deductible plans with Health Savings Accounts (HSAs) for future medical expenses.
- Middle-aged employees (40s–50s) may require comprehensive coverage, including chronic disease management, mental health services, and prescription drug coverage.
- Older employees (50+) may benefit from lower deductibles, expanded provider networks, and specialized care options, such as cardiovascular and orthopedic treatments.
2. Health Status and Medical Needs
- Employees with pre-existing conditions (e.g., diabetes, hypertension) may require lower deductibles, access to specialists, and prescription drug benefits.
- Employees who rarely seek medical care may prefer high-deductible plans (HDHPs) with lower monthly premiums.
- Employees who travel frequently may need nationwide or international provider networks for medical care.
3. Family Coverage Requirements
- Single employees may prefer lower-cost individual coverage.
- Employees with families may require dependent coverage, maternity benefits, and pediatric services.
- Businesses should assess whether to offer tiered plans that allow employees to customize their coverage based on family needs.
By analyzing employee demographics, businesses can select a plan that provides appropriate coverage while maintaining cost efficiency.
B. Budget Constraints
Managing the financial aspects of business health insurance is critical to ensuring sustainability for both employers and employees. Several cost components must be carefully evaluated:
1. Premiums
Premiums are the fixed monthly costs that employers and employees must pay to maintain coverage.
- Employers must decide how much of the premium they will cover and how much employees will contribute.
- Offering multiple plan options (e.g., HMOs, PPOs, HDHPs) allows employees to select a plan that matches their budget and healthcare needs.
- Small businesses may qualify for tax credits through the Small Business Health Options Program (SHOP) to offset premium costs.
2. Deductibles
The deductible is the amount an employee must pay out-of-pocket before the insurance begins covering costs.
- Lower deductibles generally result in higher premiums but reduce employee financial burden at the time of service.
- High-deductible health plans (HDHPs) have lower premiums but require employees to pay more out-of-pocket before insurance kicks in.
3. Copayments and Coinsurance
- Copayments (copays) are fixed amounts employees pay for services (e.g., $30 for a doctor visit).
- Coinsurance is a percentage-based payment (e.g., employees pay 20% of the total cost, and insurance covers 80%).
- Employers should evaluate cost-sharing strategies that keep healthcare affordable while maintaining financial balance.
4. Out-of-Pocket Maximums
The out-of-pocket maximum is the total amount employees must pay in a given year before insurance covers 100% of costs.
- Plans with low out-of-pocket maximums provide greater financial protection but often come with higher premiums.
- High-deductible plans may have higher out-of-pocket limits, making them riskier for employees with frequent medical needs.
5. Employer Contribution Strategy
Employers should determine:
✔ What percentage of premiums they will cover (industry standard ranges from 50% to 80%).
✔ Whether to offer dependent coverage and how much of the cost will be subsidized.
✔ How to structure benefits to maximize tax savings, such as offering HSAs, FSAs, or wellness incentives.
By balancing premiums, deductibles, and out-of-pocket costs, employers can create affordable and sustainable health insurance plans for their workforce.
C. Network Availability
The network of healthcare providers available in a health plan is a crucial factor in determining employee satisfaction and accessibility to care.
1. In-Network vs. Out-of-Network Coverage
- In-network providers have agreements with the insurance carrier to offer services at discounted rates, reducing employee costs.
- Out-of-network providers do not have contracts with the insurer, leading to higher costs for employees.
- Employers should prioritize plans with extensive in-network providers to minimize out-of-pocket expenses for employees.
2. Geographic Accessibility
- Local businesses should ensure their insurance plan covers hospitals and clinics within commuting distance of employees.
- National or remote businesses should select a plan with a nationwide provider network.
- Businesses with international employees or frequent travelers should consider global health insurance options.
3. Specialist Access
- Plans with narrow networks may limit employee access to specialists such as cardiologists, endocrinologists, or mental health professionals.
- Preferred Provider Organizations (PPOs) allow employees to see specialists without referrals, offering greater flexibility.
- Health Maintenance Organizations (HMOs) require referrals for specialist visits, potentially delaying necessary care.
4. Telemedicine and Digital Health Services
- Many modern health plans now include telehealth services, enabling employees to consult doctors remotely for minor conditions.
- Employers should consider plans that offer 24/7 virtual healthcare access, especially for remote or hybrid workforces.
5. Pharmacy Network Coverage
- Businesses should evaluate whether the plan covers essential prescription drugs at affordable copays.
- Some plans offer mail-order pharmacy services, which can reduce costs for employees requiring long-term medications.
IV. Benefits of Offering Health Insurance
Providing health insurance as part of an employee benefits package offers significant advantages to businesses. Beyond fulfilling legal obligations, offering health coverage improves employee well-being, increases workplace productivity, and enhances a company’s reputation as an employer of choice. Below are three key benefits businesses gain from offering health insurance to their workforce.
A. Tax Advantages
One of the primary financial benefits of offering health insurance is the tax incentives available to employers. These incentives help offset costs, making it more affordable for businesses—especially small and mid-sized companies—to provide comprehensive coverage.
1. Tax Deductions for Employer Contributions
- Employers can deduct the cost of health insurance premiums as a business expense, reducing overall taxable income.
- This applies to both fully insured and self-funded health plans.
2. Small Business Health Care Tax Credit
For small businesses, the Small Business Health Care Tax Credit helps offset up to 50% of premium costs for businesses that qualify.
Eligibility Requirements:
✔ The business must have fewer than 25 full-time equivalent (FTE) employees.
✔ The average annual employee salary must be $56,000 or less (as of 2023).
✔ The employer must pay at least 50% of employee premiums.
✔ The health insurance plan must be purchased through the Small Business Health Options Program (SHOP) Marketplace.
3. Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs)
Employers can offer tax-advantaged HSAs or FSAs, which provide financial benefits to both employees and businesses:
- HSA Contributions Are Tax-Free – Employers who contribute to employees’ Health Savings Accounts can deduct these contributions from their taxable income.
- FSAs Reduce Payroll Taxes – Employer and employee contributions to Flexible Spending Accounts reduce the amount of taxable income, lowering payroll taxes.
4. Payroll Tax Savings
- Employees’ contributions to employer-sponsored health insurance plans are pre-tax, reducing their taxable income.
- Employers pay lower payroll taxes because taxable wages are reduced.
By leveraging tax deductions, credits, and savings, businesses can significantly reduce the cost of offering health insurance, making it a financially viable investment.
B. Enhanced Employee Satisfaction
Offering comprehensive health insurance is one of the most effective ways to boost employee morale, job satisfaction, and workplace engagement. Employees value health benefits as a key factor in their overall compensation package, making it a powerful tool for increasing workplace happiness.
1. Reduced Financial Stress for Employees
- Medical expenses are a leading cause of financial stress among employees.
- Access to affordable health insurance helps reduce this burden, allowing employees to focus on their work instead of worrying about healthcare costs.
2. Improved Physical and Mental Health
- Employees with health insurance are more likely to seek preventive care, reducing long-term medical expenses and improving their overall well-being.
- Access to mental health services and telemedicine options helps employees manage stress, anxiety, and burnout, leading to higher productivity and job performance.
3. Higher Workplace Engagement
- Employees who feel valued and supported are more engaged, motivated, and committed to their work.
- A well-structured health benefits package reinforces a company’s commitment to employee well-being.
4. Increased Productivity and Lower Absenteeism
- Health insurance promotes regular check-ups and early disease detection, helping employees stay healthier and work more efficiently.
- Preventive care reduces sick days, minimizing disruptions in business operations.
By investing in employee health, businesses create a happier, healthier, and more engaged workforce, which translates into better performance and higher productivity.
C. Improved Recruitment and Retention
A strong health benefits package is a key differentiator in today’s competitive job market. Employers who offer comprehensive health coverage are more likely to attract top talent and retain their most valuable employees.
1. Competitive Advantage in Hiring
- Job seekers prioritize health benefits when choosing between job offers.
- Companies with robust health insurance plans stand out from competitors who offer minimal or no coverage.
- Many employees are willing to accept slightly lower salaries if they receive comprehensive health benefits.
2. Higher Employee Retention Rates
- Employees who receive good health insurance are more likely to stay with their employer.
- Companies with strong benefits packages experience lower turnover rates, reducing the costs associated with hiring and training new employees.
- Losing a skilled employee can cost up to 33% of their annual salary, making health insurance an effective investment in employee retention.
3. Attracting Skilled Professionals
- In industries where highly skilled professionals are in demand, offering health benefits is crucial for recruitment success.
- Many professionals expect employer-sponsored health insurance and may reject job offers that do not include comprehensive coverage.
4. Employer Brand and Reputation
- Companies that offer high-quality health benefits enhance their reputation as an employee-centric workplace.
- Positive employer branding helps attract more applicants and improve employee word-of-mouth referrals.
By offering competitive health benefits, businesses can build a stronger, more stable workforce, reducing turnover and making talent acquisition easier.
V. Challenges in Providing Health Insurance
While offering health insurance is a valuable investment in employee well-being, it also comes with significant challenges for employers. Rising healthcare costs, administrative complexities, and constantly evolving regulations can create financial and logistical hurdles. To effectively manage employee health benefits, businesses must understand these challenges and develop strategic solutions to overcome them.
A. Rising Premium Costs
1. The Financial Strain of Increasing Premiums
One of the most pressing challenges businesses face is the rising cost of health insurance premiums. Over the past decade, healthcare costs have consistently increased, making it more expensive for employers to offer comprehensive coverage.
- According to industry data, health insurance premiums have risen faster than wages and inflation, creating financial pressure on companies.
- Small businesses are particularly vulnerable because they lack the negotiating power of larger corporations when dealing with insurance providers.
2. Factors Driving the Increase in Premiums
Several factors contribute to the escalating cost of health insurance:
✔ Medical Inflation – Advances in medical technology, prescription drugs, and treatment methods drive up overall healthcare costs.
✔ Chronic Disease Prevalence – Conditions like diabetes, heart disease, and obesity require ongoing treatment, increasing long-term healthcare expenditures.
✔ Aging Workforce – Older employees generally have higher healthcare utilization rates, leading to increased claims and higher premiums.
✔ Increased Demand for Mental Health Services – The demand for mental health care and behavioral therapy has grown, adding to insurance costs.
✔ Provider Consolidation – Mergers between hospitals and healthcare providers reduce competition, enabling higher pricing for services.
3. Strategies for Controlling Premium Costs
To mitigate rising premiums, employers can implement cost-saving strategies while maintaining quality benefits for employees:
✔ Wellness Programs – Encouraging preventive care, fitness programs, and mental health initiatives can reduce long-term healthcare expenses.
✔ High-Deductible Health Plans (HDHPs) with Health Savings Accounts (HSAs) – These plans offer lower premiums while allowing employees to save pre-tax funds for medical expenses.
✔ Self-Funded or Level-Funded Plans – Businesses with a stable workforce can explore alternative funding models that provide cost flexibility.
✔ Negotiating with Insurance Providers – Partnering with brokers or benefits consultants can help businesses secure better rates from insurance carriers.
✔ Telemedicine and Virtual Healthcare – Providing telehealth options reduces unnecessary ER visits and in-person consultations, cutting down medical expenses.
By proactively managing costs, businesses can offer affordable, sustainable health benefits without compromising employee well-being.
B. Administrative Burden
1. Complexity of Managing Health Insurance Plans
Administering health insurance requires significant effort, from plan selection and enrollment to compliance and employee support. The complexity increases as companies grow and regulations evolve.
2. Key Administrative Challenges
Employers face multiple administrative burdens when managing health insurance plans:
✔ Plan Selection and Renewal – Choosing the right health plan requires evaluating costs, provider networks, and coverage options annually.
✔ Enrollment and Employee Support – HR teams must assist employees with understanding benefits, selecting plans, and resolving coverage issues.
✔ Claims Management – Employers using self-funded plans must oversee claim approvals, reimbursements, and disputes.
✔ Data Privacy Compliance – Health insurance plans must comply with HIPAA regulations, ensuring that employee health information remains confidential.
✔ Billing and Premium Payments – Businesses must track premium contributions, payroll deductions, and billing accuracy.
3. Solutions for Reducing Administrative Workload
To streamline health insurance administration, businesses can adopt technology-driven solutions and external support:
✔ HR and Benefits Software – Platforms like Zenefits, Gusto, and ADP automate enrollment, payroll deductions, and compliance tracking.
✔ Third-Party Administrators (TPAs) – Businesses using self-funded plans can outsource administrative tasks to TPAs for efficient claims processing.
✔ Employee Education Initiatives – Providing clear benefits guides, FAQs, and online resources reduces the number of employee inquiries.
✔ Broker and Consultant Partnerships – Insurance brokers help negotiate better plans, manage compliance, and simplify plan administration.
By leveraging automation and expert support, businesses can reduce the administrative burden, allowing HR teams to focus on employee engagement and productivity.
C. Keeping Up with Regulatory Changes
1. The Challenge of Evolving Healthcare Laws
Health insurance regulations frequently change, requiring businesses to stay informed to maintain compliance and optimize employee benefits.
2. Key Regulations Affecting Business Health Insurance
✔ Affordable Care Act (ACA) – Employers with 50+ employees must provide affordable, minimum essential coverage to avoid penalties.
✔ COBRA (Consolidated Omnibus Budget Reconciliation Act) – Businesses with 20+ employees must offer continuation coverage for employees who leave the company.
✔ ERISA (Employee Retirement Income Security Act) – Requires employers to provide clear information about health plan benefits and rules.
✔ HIPAA (Health Insurance Portability and Accountability Act) – Mandates data security for employee health records and ensures portability of coverage.
✔ State-Level Regulations – Many states impose additional requirements on employer-sponsored health plans, including mandated benefits and coverage standards.
3. Staying Compliant and Adaptable
Employers must take proactive measures to stay ahead of regulatory updates and maintain legally compliant health benefits:
✔ Regular Compliance Audits – Conducting internal benefits plan reviews ensures that health coverage aligns with federal and state laws.
✔ HR and Legal Training – Keeping HR teams informed about policy changes reduces the risk of compliance violations.
✔ Partnering with Benefits Consultants – Working with industry experts helps businesses navigate complex regulations and implement the best solutions.
✔ Monitoring Government Updates – Employers should follow IRS, Department of Labor (DOL), and Health and Human Services (HHS) guidelines for policy changes.
✔ Flexible Plan Design – Businesses should maintain adaptive health plans that can be adjusted based on regulatory shifts.
By staying informed and proactive, businesses can avoid legal penalties, optimize employee benefits, and maintain compliance in an ever-changing healthcare landscape.
VI. Future Trends in Business Health Insurance
The landscape of business health insurance is evolving rapidly, influenced by technological advancements, changing workforce expectations, and a growing emphasis on preventive care. To remain competitive and cost-effective, companies must adapt their health benefits strategies to align with emerging trends. Below are the key future trends shaping business health insurance and their impact on employers and employees.
A. Telemedicine Integration
1. The Rise of Telemedicine in Employee Health Benefits
Telemedicine has transformed how employees access healthcare services, offering a cost-effective, convenient, and efficient alternative to traditional in-person visits. Many businesses are now incorporating virtual healthcare services into their health insurance plans to improve employee well-being while reducing overall healthcare expenses.
2. Benefits of Telemedicine for Businesses and Employees
For Employers:
✔ Lower Healthcare Costs – Virtual consultations are cheaper than in-person visits, reducing overall medical claims and insurance premiums.
✔ Reduced Employee Absenteeism – Employees can access medical care without leaving the workplace or taking excessive time off.
✔ Improved Productivity – Quick access to doctors minimizes disruptions in workflow and allows employees to address health concerns efficiently.
For Employees:
✔ Convenience and Accessibility – Employees can consult doctors remotely from home or work, eliminating long wait times and unnecessary travel.
✔ Expanded Access to Specialists – Telehealth allows workers to connect with mental health professionals, nutritionists, and chronic disease specialists without geographical barriers.
✔ Enhanced Preventive Care – Employees are more likely to seek timely medical attention, preventing minor health concerns from escalating.
3. Telehealth Services Being Integrated into Health Plans
Employers are incorporating various telemedicine services into their business health insurance plans, such as:
- 24/7 Virtual Doctor Consultations – Employees can access primary care providers, specialists, and urgent care services via video or phone.
- Remote Mental Health Support – Virtual therapy sessions and counseling programs address stress, anxiety, and workplace burnout.
- Chronic Disease Management – Telemedicine solutions allow diabetic, hypertensive, and cardiac patients to monitor their health remotely.
- Digital Prescription Services – Employees can receive prescriptions electronically, reducing the need for physical pharmacy visits.
4. The Future of Telemedicine in Employer Health Plans
✔ AI-Driven Virtual Health Assistants – AI-powered chatbots and virtual assistants will help employees schedule appointments, analyze symptoms, and receive medical advice.
✔ Wearable Health Technology Integration – Devices like smartwatches and fitness trackers will sync with telehealth platforms to provide real-time health monitoring.
✔ Expanded Insurance Coverage – More health plans will cover telemedicine services as standard benefits, making virtual healthcare even more accessible.
Telemedicine is becoming a core component of modern business health insurance, enabling companies to offer quality healthcare while controlling costs.
B. Wellness Programs
1. The Growing Importance of Workplace Wellness Initiatives
Workplace wellness programs are gaining traction as businesses recognize the long-term benefits of investing in employee health. By encouraging preventive care, fitness, and mental well-being, wellness initiatives can reduce healthcare costs, improve productivity, and enhance overall employee satisfaction.
2. Benefits of Implementing Wellness Programs
For Employers:
✔ Reduced Healthcare Costs – Healthy employees are less likely to develop chronic illnesses, lowering insurance claims and premiums.
✔ Increased Employee Productivity – Improved physical and mental well-being leads to higher concentration levels and better work performance.
✔ Stronger Employee Retention and Engagement – Workers value wellness benefits, increasing job satisfaction and loyalty.
For Employees:
✔ Better Health Outcomes – Wellness initiatives promote exercise, healthy eating, and stress management, reducing the risk of chronic diseases.
✔ Improved Mental Well-Being – Programs focused on meditation, therapy, and stress relief help employees maintain emotional resilience.
✔ Financial Savings – Employees spend less on medical expenses, prescriptions, and doctor visits when they adopt healthier lifestyles.
3. Key Wellness Initiatives Being Adopted by Businesses
Employers are increasingly incorporating comprehensive wellness programs that include:
- On-Site and Virtual Fitness Programs – Access to gyms, yoga classes, and guided workouts to encourage physical activity.
- Nutritional Counseling and Healthy Eating Initiatives – Providing employees with dietary guidance, meal plans, and healthy snacks.
- Mental Health and Stress Management Programs – Offering therapy sessions, mindfulness workshops, and Employee Assistance Programs (EAPs).
- Preventive Health Screenings and Vaccination Clinics – Encouraging early detection of medical conditions through regular check-ups.
- Financial Wellness Support – Providing education on medical savings plans, insurance literacy, and financial planning for healthcare expenses.
4. The Future of Workplace Wellness Programs
✔ AI-Powered Wellness Coaching – Personalized digital coaching using AI-driven health recommendations.
✔ Incentive-Based Wellness Programs – Employers rewarding employees with discounted premiums or financial incentives for meeting health goals.
✔ Genetic and Personalized Health Assessments – Employees receiving DNA-based health insights to optimize preventive care strategies.
Wellness programs will continue to evolve as a key pillar of business health insurance, promoting preventive healthcare and long-term cost reduction.
C. Personalized Plan Options
1. The Shift Toward Customizable Health Plans
A one-size-fits-all approach to health insurance is becoming outdated. Employees have diverse medical needs, making customizable health plan options a growing trend in employer-sponsored insurance.
2. Benefits of Offering Personalized Health Plans
✔ Greater Employee Satisfaction – Workers appreciate having choices that align with their healthcare needs and financial situations.
✔ Cost Efficiency for Employers – Customizable plans allow businesses to control costs while offering competitive benefits.
✔ Improved Healthcare Utilization – Employees use their benefits more effectively when they have coverage options tailored to their lifestyle.
3. How Employers Are Personalizing Health Insurance
- Flexible Tiered Plans – Employees can choose between multiple coverage levels (e.g., basic, standard, or premium options).
- Voluntary Benefits – Businesses offer add-on benefits like dental, vision, life insurance, and disability coverage, allowing employees to select only what they need.
- Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) – Employees can set aside pre-tax money for healthcare expenses, giving them greater control over medical spending.
- Personalized Preventive Care Programs – Tailored plans that focus on high-risk employees (e.g., those with chronic illnesses) to provide proactive disease management.
- Digital Benefits Portals – Employers provide online platforms where employees can customize their coverage, track claims, and access wellness resources.
4. The Future of Personalized Business Health Insurance
✔ AI and Data-Driven Plan Recommendations – Employees will receive customized coverage suggestions based on their health history and lifestyle.
✔ More Flexible Employer Contributions – Companies will provide healthcare stipends or defined contributions, allowing employees to spend them on plans of their choice.
✔ Blockchain-Based Health Benefits – Secure and transparent management of healthcare data for easier claim processing and fraud prevention.
Personalized health insurance plans will continue to gain traction, ensuring that employees receive the most relevant and cost-effective coverage.
















Content that may interest you