Employee health insurance
Employee health insurance is a critical component of the modern workplace, offering numerous benefits to both employers and employees. For employers, providing health coverage can enhance employee satisfaction, reduce turnover, and increase productivity. Employees, in turn, gain access to essential medical services, financial protection against high medical costs, and overall peace of mind. Understanding the intricacies of employee health insurance is vital for organizations aiming to attract and retain top talent while ensuring the well-being of their workforce.
I. Overview of Employee Health Insurance
A. Definition and Importance
What is Employee Health Insurance?
Employee health insurance is a form of group health coverage that employers provide to their workers as part of a benefits package. This type of insurance helps employees access medical services while reducing their financial burden. In many cases, employers subsidize a portion of the premium costs, making health coverage more affordable for their workforce.
A typical employee health insurance plan includes:
- Medical coverage for doctor visits, hospital stays, and surgeries.
- Preventive care such as vaccinations, screenings, and annual check-ups.
- Prescription drug benefits to lower the cost of medications.
- Mental health and wellness services, including therapy and counseling.
- Specialized care options, such as maternity, dental, and vision coverage.
Why is Employee Health Insurance Important?
For Employers:
Offering health insurance is not just a benefit—it is a strategic tool for businesses to attract and retain top talent. Here’s why:
- Boosts Employee Satisfaction & Retention – Employees with health coverage are more likely to stay with their employer, reducing turnover costs.
- Enhances Productivity – Healthy employees take fewer sick days, leading to better workplace efficiency.
- Tax Advantages – Employers may receive tax incentives or deductions for providing health benefits.
- Compliance with Regulations – In some countries, businesses are required by law to provide health insurance to employees.
For Employees:
Having access to employer-sponsored health insurance significantly improves employees' well-being and financial stability. Key benefits include:
- Financial Protection – Reduces out-of-pocket expenses for major medical treatments.
- Access to Quality Healthcare – Employees can visit doctors, specialists, and hospitals without excessive financial stress.
- Peace of Mind – Knowing they are covered in case of illness or emergencies.
- Family Coverage – Many plans allow employees to include dependents, ensuring family members also receive medical care.
B. Historical Context
The Evolution of Employer-Sponsored Health Insurance in the U.S.
Employee health insurance in the U.S. has undergone significant transformations over the past century. The concept of employer-sponsored health benefits emerged as a response to economic and political factors, shaping the way businesses provide healthcare today.
1. The Early 1900s: The Birth of Employer-Sponsored Insurance
- In the early 20th century, healthcare was primarily out-of-pocket, meaning individuals had to pay for medical services directly.
- During the Great Depression (1929–1939), hospitals began offering prepaid plans to ensure a steady flow of patients. This led to the development of Blue Cross and Blue Shield, two of the first health insurance providers.
2. World War II and the Rise of Employer-Based Insurance
- During World War II (1941–1945), the U.S. government imposed wage controls to prevent inflation.
- Since employers could not increase wages, they started offering health benefits as an alternative form of compensation.
- The government later exempted employer-sponsored health insurance from taxes, making it a more attractive benefit for both employers and employees.
3. Post-War Expansion and the 1960s-1980s Healthcare Boom
- In 1965, the U.S. government established Medicare and Medicaid, expanding healthcare access to the elderly and low-income individuals.
- Private employers continued offering health insurance, and by the 1970s, most full-time employees had access to employer-sponsored coverage.
- The Employee Retirement Income Security Act (ERISA) of 1974 introduced federal regulations to protect employees' benefits.
4. The 1990s-2000s: Rising Costs and Managed Care
- Healthcare costs surged in the 1990s, leading to the rise of Managed Care Plans like Health Maintenance Organizations (HMOs) and Preferred Provider Organizations (PPOs).
- Employers sought ways to control costs by offering High-Deductible Health Plans (HDHPs) paired with Health Savings Accounts (HSAs).
5. The Affordable Care Act (ACA) and Modern Reforms
- The Affordable Care Act (ACA), enacted in 2010, introduced the employer mandate, requiring large businesses to offer health insurance to full-time employees.
- The ACA also standardized minimum essential benefits, ensuring that employer-sponsored plans provided comprehensive coverage.
- In recent years, telemedicine and digital health solutions have become popular additions to employee health benefits.
Key Legislative Milestones Impacting Employee Health Coverage
| Legislation | Year | Impact on Employee Health Insurance |
| Social Security Act | 1935 | Laid the foundation for Medicare & Medicaid. |
| IRS Tax Exemption on Employer Health Benefits | 1943 | Made employer-sponsored insurance tax-free, increasing adoption. |
| Employee Retirement Income Security Act (ERISA) | 1974 | Established regulations for employer-sponsored benefit plans. |
| Health Insurance Portability and Accountability Act (HIPAA) | 1996 | Improved access to health insurance and protected patient data. |
| Affordable Care Act (ACA) | 2010 | Introduced the employer mandate and expanded coverage options. |
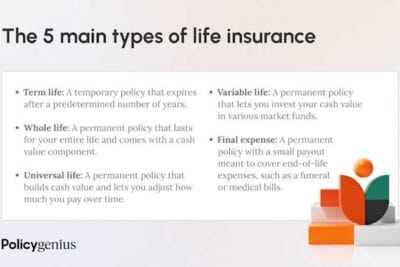
II. Types of Employee Health Insurance Plans
Selecting the right health insurance plan is a crucial decision for both employers and employees. Each type of plan offers different levels of flexibility, costs, and network restrictions. Below is an in-depth analysis of the most common employee health insurance plans, outlining their characteristics, benefits, and potential drawbacks.
A. Health Maintenance Organizations (HMOs)
Characteristics and Structure
A Health Maintenance Organization (HMO) is a type of health insurance plan that focuses on providing comprehensive medical care through a network of contracted healthcare providers. HMOs emphasize preventive care and typically require members to choose a Primary Care Physician (PCP) who coordinates all healthcare services.
Key features of an HMO plan:
- Network Restrictions: Members must use doctors, hospitals, and specialists within the plan’s approved network.
- Primary Care Physician (PCP) Requirement: A PCP acts as the main doctor and provides referrals to specialists.
- Lower Costs: Premiums and out-of-pocket expenses (e.g., copays) are generally lower compared to other plans.
- Preventive Care Focus: HMOs encourage routine check-ups, screenings, and vaccinations to prevent serious illnesses.
Advantages of HMOs
✔ Lower Premiums and Out-of-Pocket Costs compared to other insurance plans.
✔ Emphasis on Preventive Care can help reduce long-term medical expenses.
✔ Coordinated Healthcare ensures streamlined treatments and fewer redundant medical procedures.
Disadvantages of HMOs
✖ Limited Provider Network – Out-of-network care is generally not covered, except in emergencies.
✖ Referral Requirements – To see a specialist, members must first obtain approval from their PCP.
✖ Less Flexibility – Members cannot freely choose healthcare providers outside the network.
B. Preferred Provider Organizations (PPOs)
Features and Network Flexibility
A Preferred Provider Organization (PPO) is a type of health plan that offers more flexibility in choosing healthcare providers, both in and out of the network. Unlike HMOs, PPOs do not require referrals to see specialists.
Key features of a PPO plan:
- Larger Network of Providers: Members can receive care from both in-network and out-of-network doctors and hospitals.
- No Referral Requirement: Employees can visit specialists without prior approval from a PCP.
- Higher Costs for Out-of-Network Services: PPOs cover out-of-network care, but at a higher cost to the insured.
Pros of PPOs
✔ More Freedom to Choose Providers – Employees can visit any doctor or specialist without needing a referral.
✔ Out-of-Network Coverage – Unlike HMOs, PPOs partially cover out-of-network care.
✔ Ideal for Employees Who Travel Frequently – PPOs offer more flexibility for those who may need healthcare services outside their local area.
Cons of PPOs
✖ Higher Premiums – PPO plans are more expensive compared to HMOs.
✖ Higher Deductibles and Copays – Employees may have to pay more upfront before insurance covers expenses.
✖ Complex Billing Process – Out-of-network providers may require employees to file claims manually.
C. Exclusive Provider Organizations (EPOs)
Definition and Network Limitations
An Exclusive Provider Organization (EPO) is similar to an HMO in that it requires members to use a network of approved providers but functions like a PPO by not requiring referrals to see specialists.
Key features of an EPO plan:
- Network-Only Coverage: Employees must use doctors, specialists, and hospitals within the plan’s network.
- No PCP or Referral Requirement: Members can visit specialists directly without needing a PCP's approval.
- Lower Premiums than PPOs: EPOs are more affordable than PPOs but often come with higher deductibles.
Benefits of EPOs
✔ No Referrals Needed – Employees have direct access to specialists.
✔ Lower Costs Compared to PPOs – Premiums and out-of-pocket costs are typically more manageable.
✔ Simplified Coverage – Employees don’t have to coordinate referrals with a PCP.
Drawbacks of EPOs
✖ No Out-of-Network Coverage – Unless it’s an emergency, employees must stay within the provider network.
✖ Smaller Provider Network – EPOs may have fewer healthcare providers compared to PPOs.
✖ Higher Deductibles – Employees may need to pay more upfront before coverage kicks in.
D. Point of Service (POS) Plans
Combination of HMO and PPO Elements
A Point of Service (POS) plan is a hybrid of HMO and PPO plans, offering a balance of cost control and provider flexibility. Employees must choose a Primary Care Physician (PCP) but have the option to see out-of-network providers at a higher cost.
Key features of a POS plan:
- PCP Requirement: Employees need a designated Primary Care Physician to manage their care.
- Specialist Referrals Needed: Like an HMO, members need referrals to see specialists.
- Out-of-Network Coverage Available: Employees can see out-of-network doctors but at higher costs.
Strengths of POS Plans
✔ More Flexibility Than HMOs – Employees can go out-of-network if needed.
✔ Lower Costs for In-Network Care – Employees pay less when they stick to the plan’s network.
✔ Encourages Preventive Care – Requires a PCP who manages overall health.
Weaknesses of POS Plans
✖ Higher Costs for Out-of-Network Care – Deductibles and copays are significantly higher when using non-network providers.
✖ More Paperwork – Employees may need to submit claims when seeing out-of-network doctors.
✖ Referral Requirement – Similar to an HMO, employees must get referrals for specialist visits.
E. High-Deductible Health Plans (HDHPs) with Health Savings Accounts (HSAs)
Explanation of HDHPs and HSAs
A High-Deductible Health Plan (HDHP) is a type of health insurance that has lower premiums but requires employees to pay higher deductibles before coverage begins. Many HDHPs are paired with a Health Savings Account (HSA), which allows employees to save pre-tax dollars for medical expenses.
Key features of an HDHP:
- Higher Deductibles: Employees must pay a significant amount out-of-pocket before insurance starts covering expenses.
- Lower Monthly Premiums: In exchange for a higher deductible, employees pay less in premiums.
- HSA Eligibility: Employees can contribute tax-free funds into an HSA for future medical costs.
Potential Benefits of HDHPs with HSAs
✔ Lower Monthly Premiums – Helps employees save money on regular insurance costs.
✔ HSA Tax Advantages – Contributions are tax-free, grow tax-free, and can be used tax-free for medical expenses.
✔ Encourages Cost-Conscious Healthcare Decisions – Employees are more mindful of their medical spending.
Considerations and Downsides
✖ High Out-of-Pocket Costs – Employees may struggle with high deductibles.
✖ Not Ideal for Frequent Medical Needs – Employees who need regular doctor visits or prescriptions may find HDHPs expensive.
✖ Requires Financial Planning – Employees must actively manage HSA contributions to maximize benefits.
III. Key Components of Employee Health Insurance
Understanding the key components of employee health insurance is essential for both employers and employees to make informed decisions. These components determine how much employees will pay for healthcare services, how costs are shared between employers and workers, and how financial protection is provided. Below is a detailed breakdown of the fundamental elements of a health insurance plan.
A. Premiums
Definition and Factors Influencing Cost
A premium is the amount an employee pays monthly, quarterly, or annually to maintain their health insurance coverage. This cost is required regardless of whether the insured individual uses medical services.
Factors that influence the cost of premiums:
- Type of Plan Chosen – PPOs and POS plans usually have higher premiums than HMOs and EPOs.
- Employer Contribution – The more an employer covers, the lower the premium for the employee.
- Coverage Level – Plans with lower deductibles and copays tend to have higher premiums.
- Employee’s Age and Health Status – Older employees or those with pre-existing conditions may have higher insurance costs.
- Geographic Location – Healthcare costs vary depending on the state, city, or region.
Employer vs. Employee Contributions
Most employer-sponsored health insurance plans involve a cost-sharing arrangement:
- Employer Contribution: Many companies subsidize a significant portion of the premium, making coverage more affordable for employees.
- Employee Contribution: Employees pay the remaining portion of the premium, usually deducted from their paycheck before taxes, which lowers taxable income.
Employers often cover between 50% and 80% of the total premium costs, but this varies based on company policies and industry standards.
B. Deductibles
Explanation and Impact on Out-of-Pocket Expenses
A deductible is the amount an employee must pay out-of-pocket for healthcare services before the insurance plan starts covering costs.
- Low-deductible plans have higher premiums but start covering medical costs sooner.
- High-deductible plans (HDHPs) have lower premiums but require employees to pay more upfront before insurance benefits apply.
For example, if an employee has a $1,500 deductible, they must pay $1,500 in medical expenses before the insurance covers additional costs, except for preventive services, which are usually covered regardless of the deductible.
Strategies for Managing High Deductibles
- Health Savings Accounts (HSAs) and Flexible Spending Accounts (FSAs) – Employees can contribute pre-tax dollars to cover deductible expenses.
- Choosing a Plan Based on Healthcare Needs – Employees who rarely visit the doctor may benefit from a high-deductible plan, while those with chronic conditions may prefer a lower deductible plan.
- Employer Contributions to HSAs – Some employers provide HSA contributions to help offset high deductibles.
C. Copayments and Coinsurance
Differences Between Copays and Coinsurance
| Term | Definition | How It Works |
| Copayment (Copay) | A fixed amount the employee pays for medical services or prescriptions. | Example: A $30 copay for a doctor visit means the employee pays $30, and insurance covers the rest. |
| Coinsurance | A percentage of the total medical cost that the employee pays. | Example: If the coinsurance is 20%, the employee pays 20% of a $1,000 procedure ($200), and insurance covers the remaining 80%. |
How They Affect Healthcare Utilization
- Lower copays encourage employees to seek medical care because they know exactly how much they will pay upfront.
- Coinsurance can make high-cost treatments more expensive, leading employees to delay necessary medical care.
- Employees should compare copay and coinsurance amounts when selecting a plan to understand potential out-of-pocket costs.
D. Out-of-Pocket Maximums
Definition and Importance for Financial Protection
An out-of-pocket maximum (OOPM) is the highest amount an employee must pay in a given year before the insurance plan covers 100% of additional medical costs.
Once the OOPM is reached, the insurance covers all eligible healthcare expenses, including hospital visits, surgeries, and specialist consultations.
For example, if an employee has an $8,000 out-of-pocket maximum, once they spend $8,000 on deductibles, copays, and coinsurance, the insurance covers 100% of additional costs for the rest of the year.
Annual Limits and What Expenses Apply
- Deductibles, copays, and coinsurance contribute to the out-of-pocket maximum.
- Premium payments DO NOT count toward the OOPM.
- Different plans have different limits – lower-cost plans generally have higher OOPMs, while higher-premium plans may have lower OOPMs.
IV. Legal and Regulatory Considerations
Health insurance is subject to strict regulations that ensure fair access, employer compliance, and financial protection for employees. Understanding these regulations is essential for businesses to avoid penalties and provide adequate coverage. The following are three key laws that impact employer-sponsored health insurance in the United States.
A. Affordable Care Act (ACA) Requirements
The Affordable Care Act (ACA), signed into law in 2010, introduced sweeping reforms to the U.S. healthcare system, including mandatory employer-sponsored health insurance for certain businesses.
Employer Mandate and Coverage Standards
Under the Employer Shared Responsibility Provision, the ACA requires large employers (50+ full-time employees) to provide affordable, minimum essential coverage (MEC) to at least 95% of their full-time workforce.
Key coverage requirements under ACA:
- Essential Health Benefits (EHBs) – Employer-sponsored plans must cover a set of minimum benefits, including:
- Preventive services (vaccinations, screenings, annual check-ups)
- Hospitalization
- Emergency services
- Prescription drugs
- Maternity and newborn care
- Mental health and substance abuse treatment
- Affordability Standard – Employee contributions for self-only coverage cannot exceed 9.12% of their household income (as of 2023).
- Employer Penalties for Non-Compliance – Failure to offer ACA-compliant health insurance can result in significant financial penalties (Employer Shared Responsibility Payment).
Impact on Small vs. Large Businesses
| Business Size | ACA Requirements | Penalty for Non-Compliance |
| Small Businesses (Less than 50 FTEs) | Not required to offer health insurance, but can participate in the Small Business Health Options Program (SHOP). | No penalty for not offering coverage. |
| Large Businesses (50+ FTEs) | Required to provide affordable, minimum essential health coverage. | Penalty of $2,970 per employee (if no coverage is provided). |
For small businesses, offering voluntary health insurance can still provide competitive advantages, such as tax credits through the SHOP marketplace.
B. Employee Retirement Income Security Act (ERISA)
The Employee Retirement Income Security Act (ERISA), enacted in 1974, is a federal law that sets standards for employer-sponsored health and retirement plans. ERISA ensures that employees receive fair treatment and have access to information regarding their health benefits.
Overview and Relevance to Health Plans
ERISA applies to most private-sector employer health plans and regulates:
- Plan disclosures – Employers must provide clear information about coverage, costs, and benefits.
- Fiduciary responsibilities – Employers must act in the best interest of employees when managing health benefits.
- Claims and appeals process – Employees have the right to challenge denied claims through a formal appeals process.
ERISA does not require employers to offer health insurance, but once a plan is established, it must comply with ERISA rules.
Compliance Obligations for Employers
Employers who provide health insurance must:
✔ Provide a Summary Plan Description (SPD) – A detailed document outlining plan benefits, costs, and rules.
✔ Follow Non-Discrimination Rules – Employers cannot structure plans that favor executives or high-income employees over others.
✔ Ensure Compliance with Federal Laws – ERISA works alongside ACA, COBRA, and HIPAA regulations to protect employees' healthcare rights.
Failure to comply with ERISA can result in government audits, fines, and legal action.
C. Consolidated Omnibus Budget Reconciliation Act (COBRA)
The Consolidated Omnibus Budget Reconciliation Act (COBRA), passed in 1985, grants employees the right to continue health insurance coverage after leaving a job or experiencing a qualifying life event.
Continuation Coverage Provisions
COBRA applies to private-sector employers with 20+ employees and allows eligible individuals to temporarily keep their health insurance under certain conditions.
Who is eligible for COBRA?
- Employees who lose their job (voluntary or involuntary, except for gross misconduct).
- Employees who experience a reduction in work hours that affects eligibility for health insurance.
- Spouses and dependents who lose coverage due to:
- Divorce or legal separation from the covered employee.
- Death of the covered employee.
- The employee qualifying for Medicare.
Employer Responsibilities and Employee Rights
| Requirement | Employer Obligation |
| Notification | Employers must notify eligible employees about COBRA coverage within 14 days of a qualifying event. |
| Coverage Duration | COBRA coverage lasts 18 to 36 months, depending on the qualifying event. |
| Cost Responsibility | The employee pays the full premium (including the employer’s share) plus a 2% administrative fee. |
While COBRA provides a critical safety net, it can be expensive for employees because they must cover 100% of the premium cost, making alternatives like marketplace insurance plans more attractive for some.
V. Strategies for Employers
Providing a well-structured employee health insurance plan is essential for attracting and retaining top talent. However, beyond just offering coverage, employers should focus on maximizing the value of their benefits packages, ensuring that employees understand and use their benefits effectively. Below are key strategies that businesses can implement to enhance employee satisfaction, control costs, and promote workplace wellness.
A. Designing a Competitive Benefits Package
A competitive benefits package is one of the most effective ways to attract, motivate, and retain employees. Employers must strike a balance between offering valuable healthcare options and managing costs effectively.
Assessing Employee Needs and Preferences
To design a benefits package that meets employee expectations, employers should:
- Conduct Employee Surveys – Gather feedback on what employees value most in a healthcare plan (e.g., lower deductibles, mental health support, telemedicine).
- Analyze Workforce Demographics – Consider the age, family status, and health conditions of employees. Younger employees may prioritize affordable premiums, while employees with families may need comprehensive family coverage.
- Evaluate Past Healthcare Usage – Reviewing claims data can help determine which benefits are most frequently used and which are underutilized.
Balancing Cost and Coverage Options
Employers must balance affordability with comprehensive coverage to ensure employees get valuable healthcare benefits without excessive costs.
Key considerations:
- Offering Multiple Plan Options: A tiered approach (e.g., HMO, PPO, HDHP with HSA) allows employees to choose a plan that best fits their needs.
- Employer Contribution Strategies: Employers can choose to cover a higher percentage of premiums to reduce employee costs.
- Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs): Offering tax-advantaged accounts helps employees manage out-of-pocket expenses.
- Leveraging Group Purchasing Power: Partnering with industry associations or health insurance coalitions can help negotiate lower rates with insurance providers.
By customizing the benefits package, employers can ensure that it is both cost-effective and valuable to employees.
B. Wellness Programs and Preventive Care
Implementing wellness programs and preventive care initiatives can lead to long-term savings for employers by reducing chronic illnesses, absenteeism, and healthcare costs.
Incorporating Wellness Initiatives to Reduce Costs
A well-designed corporate wellness program can help employees maintain a healthy lifestyle, reducing the likelihood of costly medical conditions such as diabetes, heart disease, and obesity.
Effective workplace wellness initiatives include:
- On-site Health Screenings – Providing free blood pressure, cholesterol, and diabetes screenings encourages early detection of health issues.
- Fitness Programs and Gym Memberships – Subsidizing gym memberships or offering on-site fitness classes helps promote an active lifestyle.
- Nutritional Guidance and Healthy Eating Initiatives – Providing healthy snacks, meal plans, and nutrition coaching improves employee well-being.
- Mental Health Support – Offering Employee Assistance Programs (EAPs) that include therapy, stress management, and mindfulness programs.
- Smoking Cessation and Substance Abuse Programs – Providing access to support groups, counseling, and medical treatments to help employees quit smoking or manage substance dependence.
Encouraging Preventive Care to Improve Health Outcomes
Preventive healthcare reduces long-term medical costs by addressing health issues before they become serious conditions.
Employers can encourage preventive care by:
- Covering 100% of Preventive Services – Many insurance plans offer free preventive services such as vaccinations, cancer screenings, and annual check-ups.
- Promoting Telemedicine and Virtual Health Visits – Employees can access medical professionals remotely, reducing time away from work.
- Providing Health Education Workshops – Educating employees on nutrition, stress management, and disease prevention improves long-term health outcomes.
By investing in preventive care, employers can reduce medical claims and create a healthier workforce.
C. Communicating Benefits to Employees
Even the most comprehensive benefits package is ineffective if employees don’t understand or use their healthcare options. Effective communication strategies ensure that employees maximize their benefits and make informed healthcare decisions.
Effective Methods for Educating Staff About Their Options
Employees often struggle to understand health insurance jargon, coverage options, and cost-sharing structures. Employers should use clear, simple, and engaging communication methods to educate their workforce.
Best practices for communicating benefits:
- Hosting Annual Benefits Meetings – Conduct in-person or virtual meetings during open enrollment periods to explain plan options.
- Providing Easy-to-Understand Benefit Guides – Creating visual, step-by-step guides that break down costs, coverage, and key terms.
- Using Real-Life Scenarios – Demonstrating how different plans work using employee case studies.
- Offering 1-on-1 Benefits Counseling – Allowing employees to meet with HR specialists or insurance providers for personalized guidance.
- Sending Regular Email Updates – Keeping employees informed about plan changes, deadlines, and wellness initiatives.
Utilizing Decision Support Tools and Resources
To help employees choose the best health insurance plan, employers can provide digital tools and resources that simplify the decision-making process.
Helpful tools include:
- Online Cost Calculators – Employees can estimate total healthcare costs based on expected medical usage.
- Comparison Charts – Clear side-by-side comparisons of plan benefits, deductibles, copays, and out-of-pocket maximums.
- Chatbots and HR Portals – Interactive platforms where employees can ask questions and receive instant answers.
- Mobile Apps for Benefits Management – Allowing employees to track claims, schedule appointments, and access virtual healthcare from their phones.
Encouraging Active Employee Participation
A well-informed employee is more likely to utilize their benefits effectively and make cost-conscious healthcare decisions. Employers can:
✔ Reward employees for attending benefits meetings or completing health risk assessments.
✔ Offer incentives for enrolling in wellness programs, such as discounted premiums or wellness stipends.
✔ Create an ongoing dialogue about healthcare benefits rather than limiting communication to open enrollment periods.
VI. Challenges and Future Trends
The landscape of employee health insurance is constantly evolving, presenting challenges that impact both employers and employees. Rising healthcare costs, the integration of digital health solutions, and shifting legislation are among the most pressing concerns. Employers must stay proactive and adaptable to ensure they offer cost-effective, comprehensive, and compliant health insurance options.
A. Rising Healthcare Costs
Factors Contributing to Increasing Premiums
The cost of healthcare continues to rise, leading to higher premiums, deductibles, and out-of-pocket expenses for both employers and employees. Several key factors drive these increasing costs:
- Medical Inflation – The rising cost of medical services, prescription drugs, and hospital care leads to higher insurance premiums.
- Increased Chronic Disease Rates – Conditions like diabetes, heart disease, and obesity require long-term, expensive treatments, increasing overall healthcare spending.
- Aging Workforce – Older employees generally require more medical care, driving up employer healthcare costs.
- Advancements in Medical Technology – While new treatments and drugs improve patient outcomes, they also come with higher price tags.
- Administrative Costs – The U.S. healthcare system has high administrative expenses related to claims processing, billing, and compliance with regulations.
- Provider Consolidation – Mergers between hospitals and healthcare providers reduce competition, allowing higher pricing for services.
- Delayed Preventive Care – Employees who skip preventive check-ups due to high costs often face more severe, expensive medical issues later on.
Strategies for Cost Containment
Employers must find ways to control rising healthcare costs without sacrificing the quality of employee benefits.
Key strategies include:
- Self-Funded Health Plans – Larger businesses can pay claims directly instead of purchasing traditional insurance, reducing administrative fees.
- Wellness Programs – Promoting preventive healthcare, fitness programs, and chronic disease management can reduce long-term medical expenses.
- High-Deductible Health Plans (HDHPs) with HSAs – Encouraging employees to enroll in HDHPs paired with Health Savings Accounts (HSAs) helps lower premium costs while allowing tax-advantaged savings for medical expenses.
- Negotiating with Providers – Employers can work with insurers, hospitals, and pharmacy benefit managers (PBMs) to negotiate better pricing.
- Telemedicine and Digital Health Solutions – Offering virtual consultations reduces the cost of doctor visits and emergency room use.
- Value-Based Healthcare Models – Instead of paying for services rendered, employers can encourage outcome-based healthcare, where providers are paid based on patient recovery and long-term health improvements.
By implementing cost-containment measures, businesses can continue to offer quality health coverage while keeping expenses manageable.
B. Telemedicine and Digital Health Solutions
Emergence and Integration into Health Plans
Telemedicine and digital health solutions have transformed healthcare delivery, providing employees with virtual access to medical professionals from their homes or workplaces.
Key developments driving telemedicine adoption:
- COVID-19 Acceleration – The pandemic forced rapid adoption of telehealth as a safe and effective way to access care.
- Legislative Support – Federal and state governments have expanded coverage and reimbursement for virtual healthcare services.
- Employer Adoption – Many companies now integrate telehealth into their health plans to reduce costs and improve employee health access.
- Wearable Health Technology – Devices like smartwatches and fitness trackers provide real-time health monitoring, supporting preventive care.
Benefits for Access and Cost Efficiency
Telemedicine offers numerous advantages for both employers and employees:
✔ Lower Costs – Virtual visits are significantly cheaper than in-person doctor visits or emergency room trips.
✔ Convenience – Employees can consult doctors from home, reducing absenteeism and improving productivity.
✔ Faster Access to Specialists – Reduces long waiting times for appointments with mental health providers, dermatologists, and other specialists.
✔ Improved Preventive Care – Regular virtual check-ups encourage early diagnosis of potential health conditions.
✔ Mental Health Support – Many telemedicine platforms offer therapy and counseling services, making mental healthcare more accessible.
✔ Chronic Disease Management – Remote monitoring tools allow diabetic, hypertensive, and cardiac patients to track their conditions without frequent doctor visits.
Challenges of Telemedicine Implementation
While telemedicine is highly beneficial, it also presents challenges:
- Regulatory Compliance – Different states have varying telehealth laws, complicating implementation for nationwide employers.
- Privacy and Data Security – Employers must ensure telemedicine services comply with HIPAA to protect employee health information.
- Digital Divide – Not all employees have reliable internet access or are comfortable using telehealth technology.
- Insurance Coverage Gaps – Some insurers limit reimbursement rates for telemedicine, making it less financially attractive for providers.
Despite these challenges, telemedicine is a growing solution that lowers costs, improves access, and enhances healthcare quality for employees.
C. Legislative Changes and Uncertainty
Potential Policy Shifts Affecting Employer-Sponsored Insurance
Healthcare regulations are constantly evolving, and future legislative changes could significantly impact employer-sponsored health insurance.
Potential changes include:
- Revisions to the Affordable Care Act (ACA) – Future administrations may modify, expand, or repeal certain ACA provisions, affecting employer mandates and tax incentives.
- Medicare Expansion – Proposals to lower the Medicare eligibility age or implement Medicare-for-All could reshape employer health coverage.
- Price Transparency Rules – Employers may be required to disclose health plan costs and negotiated rates with hospitals and insurers.
- Prescription Drug Pricing Regulations – New laws could cap drug prices, reducing employer spending on pharmacy benefits.
- Expanded Mental Health Parity Requirements – Regulations could require equal coverage for mental and physical health services.
Staying Informed and Adaptable to New Regulations
Employers must stay vigilant and adaptable to comply with healthcare law changes and ensure their benefits packages remain competitive and legally compliant.
Best practices for staying compliant:
✔ Regular Policy Reviews – Employers should assess health plan compliance with ACA, ERISA, COBRA, and HIPAA regulations.
✔ Work with Benefits Consultants – Partnering with insurance brokers or legal advisors can help businesses navigate complex legislative changes.
✔ Monitor Government Updates – Employers should follow IRS, DOL, and HHS guidelines to stay informed of new policies.
✔ Engage in Industry Advocacy – Joining business coalitions or HR organizations allows employers to influence policy discussions and stay ahead of regulatory changes.
✔ Flexible Plan Designs – Employers should maintain adaptable health insurance options to accommodate future regulatory changes.

















Content that may interest you